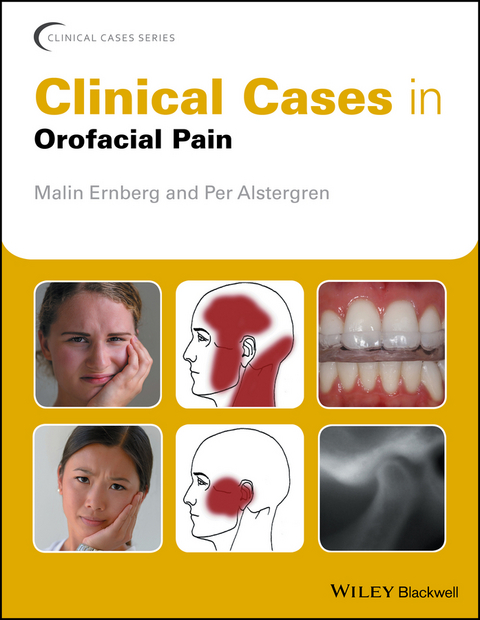
Clinical Cases in Orofacial Pain (eBook)
John Wiley & Sons (Verlag)
978-1-119-19482-8 (ISBN)
Expand your knowledge and put it into practice with this unique, case-based guide
Clinical Cases in Orofacial Pain is a valuable resource for undergraduate dental students as well as residents working towards board certification. Individual cases cover temporomandibular joint disorders, masticatory muscle disorders, headache, neuropathic pain, dental pain, tooth wear, and dystonia. Following the popular Clinical Cases series style, cases are presented with associated academic commentary, including background information, diagnostic criteria and fundamental points that might influence the diagnosis, treatment planning or management of the case.
Well-illustrated throughout, each chapter features self-assessment study questions to help foster independent learning. Clinical Cases in Orofacial Pain is an excellent primer for undergraduate dental students and an invaluable study guide for postgraduate students and residents. Dental practitioners will also want to keep this unique, case-based guide as a ready reference in their working libraries.
About the Editors
Malin Ernberg is Professor and Head of the Section for Orofacial Pain and Jaw Function at the Department of Dental Medicine, Karolinska Institutet, Sweden.
Per Alstergren is Professor and Head of the Orofacial Pain Unit at the Faculty of Odontology, Malmö University, Sweden.
About the Editors Malin Ernberg is Professor and Head of the Section for Orofacial Pain and Jaw Function at the Department of Dental Medicine, Karolinska Institutet, Sweden. Per Alstergren is Professor and Head of the Orofacial Pain Unit at the Faculty of Odontology, Malmö University, Sweden.
List of contributors
Acknowledgements
Preface
Abbreviations
Chapter 1 Introduction
Diagnostics of Orofacial Pain/TMD
Thomas List and Richard Ohrbach
Chapter 2 Temporomandibular Joint Disorders
A Joint pain
Case 1 Arthralgia
Per Alstergren
Case 2 Arthritis
Per Alstergren
B Disc disorders
Case 3 Disc displacement with reduction
Daniele Manfredini and Bachar Reda
Case 4 Disc displacement with reduction and intermittent locking
Daniele Manfredini and Massimiliano Politi
Case 5 Disc displacement without reduction with limited opening
Stanimira Kalaykova
Case 6 Disc displacement without reduction without limited opening
Stanimira Kalaykova
C Hypomobility
Case 7 Fibrous ankyloses
Tore Bjørnland
Case 8 Osseous ankyloses
Tore Bjørnland
Case 9 Coronid hyperplasia
Tore Bjørnland and Fredrik Hallmer
D Degenerative joint diseases
Case 10 Degenerative joint disease
Per Alstergren
E Systemic arthritides
Case 11 Rheumatoid arthritis
Per Alstergren
Case 12 Juvenile idiopathic arthritis
Randy Q Chron and Britt Hedenberg-Magnusson
F Other temporomandibular joint disorders
Case 13 Neoplasms (benign)
Eiro Kubota
Case 14 Neoplasm (malignant)
Eiro Kubota
Case 15 Synovial chondromatosis
Lars Eriksson and Peter Abrahamsson
Case 16 Fractures
Peter Abrahamsson and Lars Eriksson
Chapter 3 Masticatory muscle disorders
A Muscle pain
Case 17 Myalgia with limited emotional disturbance
Karina Bendixen and Peter Svensson
Case 18 Myalgia with emotional disturbance
Peter Svensson and Karina Bendixen
Case 19 Myalgia in adolescents
Claudia Restrepo and Ambra Michelotti
Case 20 Myofascial pain with referral
Paulo CR Conti
Case 21 Tendonitis
Ambra Michelotti
Case 22 Myositis
Malin Ernberg
B Other masticatory muscle disorders
Case 23 Contracture
Richard Ohrbach and Dorothy E Foigelman-Holland
Case 24 Hypertrophy
Malin Ernberg
C Masticatory muscle pain attributed to regional/generalized/ pain disorders
Case 25 Jaw-neck pain
Annemiek Rollman
Case 26 Whiplashassociated disorders/Post-traumatic neck pain
Birgitta Häggman-Henriksson and Richard Orhbach
Case 27 Fibromyalgia
Juliana Stuginski Barbosa
Chapter 4 Other orofacial pains
A Headache
Case 28 Headache attributed to TMD
Daniela AG Gonçalves
B Neuropathic pain
Case 29 Trigeminal neuralgia
Joanna Zakrewska
Case 30 Post-herpetic trigeminal neuropathy
Gary M Heir
Case 31 Post-traumatic trigeminal neuropathy
Sowmya Ananthan, Junat Khan, Vincent B Ziccardi and Rafael Benoliel
Case 32 Atypical odontalgia/persistent dentoalveolar pain
Maria Pigg and Lene Baad-Hansen
Case 33 Burning mouth syndrome
Jean-Paul Goulet and Christine Nadeau
C Dental pain and tooth wear
Case 34 Pain due to pulpitis
Natasha M Flake
Case 35 Pain due to apical periodontitis
Natasha M Flake
Case 36 Pain due to traumatic occlusion
Natasha M Flake
Case 37 Excessive tooth wear
Peter Wetselaar
D Dystonia
Case 38 Oromandibular dystonia
Merete Bakke
Chapter 1
Diagnostics of Orofacial Pain and Temporomandibular Disorders
Thomas List and Richard Ohrbach
Temporomandibular disorders (TMDs) and orofacial pain occur in about 5–12% of the adult population and in approximately 4–7% of youth and adolescents (Drangsholt, 1999; Nilsson et al., 2005; NIDCR, 2014). About half of the individuals with TMD and orofacial pain perceive a need for treatment and seek consultation (Nilsson et al., 2009; NIDCR, 2014). The consequences of TMD and orofacial pain for the patient are often a limitation in daily activities, lower quality of life, and personal suffering; the consequences for society include high economic costs for treatment and loss of productivity (NIDCR, 2014).
Although several professional groups routinely encounter patients with TMD and orofacial pain, it is the general practicing dentist who will initially manage the care of these patients. One problem is that general dentists are often unsure about diagnosing patients with TMD and orofacial pain (Tegelberg et al., 2001). Thus, there is great need for a simplified and reliable diagnostic classification with clear instructions on how to conduct the clinical examination and which questions to ask in the history to get an overall picture of the patient's difficulties and choose suitable therapy. In addition to determining diagnoses through the examination of subjective symptoms and clinical findings, it is important to assess the patient's psychosocial status, including the consequences of chronic pain, in order to reveal an overall picture of the patient. The clinical condition (Axis I) and the psychosocial assessment (Axis II) together provide the information necessary for planning and executing suitable therapy with an optimal prognosis.
Diagnostic Classifications
There are many diagnostic systems for TMD and orofacial pain (Dworkin and LeResche, 1992; de Leeuw and Klasser, 2013; Headache Classification Committee of the International Headache Society (IHS), 2013; Peck et al., 2014; Schiffman et al., 2014). Of these, the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and the American Academy of Orofacial Pain (AAOP) diagnostic criteria for TMD-related masticatory disorders have been the ones most used internationally (Dworkin and LeResche, 1992; de Leeuw and Klasser, 2013). The RDC/TMD standardized assessment of the most common TMD diagnoses and the AAOP criteria, while not as strictly defined, covered a larger range of conditions.
The RDC/TMD has been translated into more than 20 languages, and the publication that introduced it is one of the most cited in the dental literature (Dworkin and LeResche, 1992; List and Greene, 2010). After identification of some limitations of the system, the RDC/TMD was revised and the new classification system Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) (Schiffman et al., 2014) was developed, which was also incorporated into the newest edition of the AAOP guidelines (de Leeuw and Klasser, 2013), thereby bringing research and clinical practice together.
The most common temporomandibular disorders
The DC/TMD is based both on extensive multicenter clinical studies, including studies funded by the National Institutes of Health in the USA, and on international consensus conferences (Schiffman et al., 2014). It is important to point out here that the DC/TMD only covers the most commonly occurring TMD conditions. The DC/TMD is comprised of two domains: a physical Axis I and a psychosocial Axis II.
The strength of the DC/TMD Axis I protocol includes reliable and valid diagnostic criteria for the common pain-related disorders and for the intraarticular disorders. The Axis I protocol provides standardized evaluation of subjective symptoms, contains clearly defined examination methods, and utilizes specific diagnostic criteria based on the clinical findings. The Axis II protocol, a psychosocial assessment, is simplified compared with the RDC/TMD version and has two options: a brief assessment and a comprehensive set of instruments for expanded assessment. The AAOP guidelines, in parallel, include the 12 common DC/TMD diagnoses.
Less common temporomandibular disorders: the expanded taxonomy
The DC/TMD covers the most common TMD conditions for which data were readily available. This created a need to expand the taxonomy to cover less common but still clinically relevant conditions. The expanded taxonomy (Peck et al., 2014) is a consolidation of the common disorders in the DC/TMD and the less common disorders described in the fourth edition of the AAOP guidelines for TMD (De Leeuw, 2008). The expanded taxonomy defines the diagnostic criteria for the less common TMD conditions and includes a total of 37 disorders; for example, temporomandibular joint (TMJ) arthritis in cases of systemic inflammatory diseases, local TMJ arthritis, ankylosis, myositis, and orofacial dyskinesia (Peck et al., 2014) (Table 1.1). Note that while the diagnostic criteria for the less common disorders are clearly stated such that each disorder is defined without overlap, the criteria have not yet been operationalized; in addition, there is at present no information regarding the sensitivity, specificity, reliability, or validity of the diagnoses for these less common conditions (Peck et al., 2014).
Table 1.1 Expanded taxonomy of the DC/TMD
|
|
* DC/TMD with sensitivity and specificity.
Other orofacial pain conditions
Other orofacial pain conditions – such as trigeminal neuropathic pain, persistent idiopathic orofacial pain, and burning mouth syndrome – are not included in the expanded taxonomy because they are considered to be orofacial pain conditions, not TMDs. Other classification systems should be consulted in order to diagnose these conditions.
Trigeminal neuropathic pain is caused by injury or diseases of the peripheral or central somatosensory nervous system. The pain is usually constant with variations in intensity over several days, but, in rare cases, it may also occur intermittently throughout the day. Pain from normally nonpainful stimuli (such as touch, pressure, or cooling) can be a significant part of suffering in trigeminal neuropathic pain.
Treede and colleagues have published a frequently used diagnostic algorithm for neuropathic pain, proposing three levels of pain (Treede et al., 2008; Geber et al., 2009).
Possible neuropathic pain
This requires both of the following:
- i. Pain distribution is neuroanatomically plausible.
- ii.
History suggests lesion or disease of the somatosensory system.
Possible neuropathic pain indicates that the condition is not confirmed and requires further investigation.
Probable neuropathic pain
Requires (i) and (ii) with one of the following two clinical confirmatory tests being positive:
- iii. Negative or positive sensory signs confined to...
| Erscheint lt. Verlag | 1.3.2017 |
|---|---|
| Reihe/Serie | Clinical Cases (Dentistry) |
| Clinical Cases (Dentistry) | Clinical Cases (Dentistry) |
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Gesundheitsfachberufe |
| Medizin / Pharmazie ► Medizinische Fachgebiete | |
| Medizin / Pharmazie ► Zahnmedizin | |
| Schlagworte | bruxism • bruxism and orofacial pain • causes of neuropathic head pain • causes of neuropathic oral pain • dental pain causes • dental pain diagnosis • dentistry • diagnosing temporomandibular joint disorders • dystonia and orofacial pain • guide to masticatory muscle disorders • guide to temporomandibular joint disorders • <p>Orofacial pain diagnosis • masticatory muscle disorder causes • masticatory muscle disorder diagnosis • masticatory muscle disorders • masticatory muscle disorders case studies • Mundheilkunde • Mundheilkunde / Anatomie u. Physiologie • neuropathic head pain • neuropathic oral pain • neuropathic oral pain case studies • Oral Anatomy & Physiology • Oralpathologie • Oral Pathology • orofacial dystonia</p> • orofacial pain case studies • Orofacial Pain Conditions • orofacial pain syndromes • orofacial pain treatment • Orofaziale Schmerzen • Restaurative Zahnheilkunde • restorative dentistry • Temporomandibular Joint Disorders • temporomandibular joint disorders case studies • temporomandibular joint disorders causes • temporomandibular joint disorders headache • tooth wear and orofacial pain • Zahnmedizin |
| ISBN-10 | 1-119-19482-2 / 1119194822 |
| ISBN-13 | 978-1-119-19482-8 / 9781119194828 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich