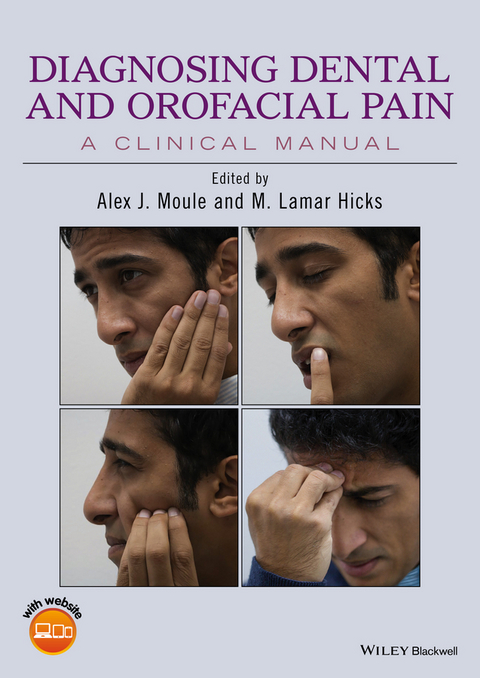
Diagnosing Dental and Orofacial Pain (eBook)
John Wiley & Sons (Verlag)
978-1-118-92499-0 (ISBN)
Diagnosing Dental and Orofacial Pain: A Clinical Manual approaches a complex topic in a uniquely practical way. This text offers valuable advice on ways to observe and communicate effectively with patients in pain, how to analyze a patients' pain descriptions, and how to provide a proper diagnosis of orofacial pain problems that can arise from a myriad of sources-anywhere from teeth, joint and muscle pain, and paranasal sinuses to cluster headaches, neuralgias, neuropathic pain and viral infections.
- Helps the student and practitioner understand the diagnostic process by addressing the exact questions that need to be asked and then analyzing verbal and non-verbal responses to these
- Edited by experts with decades of clinical and teaching experience, and with contributions from international specialists
- Companion website provides additional learning materials including videos, case studies and further practical tips for examination and diagnosis
- Includes numerous color photographs and illustrations throughout to enhance text clarity
Alex J. Moule is an Associate Professor and Discipline Lead in Endodontics at the School of Dentistry, University of Queensland, Brisbane, Queensland, Australia.
M. Lamar Hicks is Clinical Professor, Deans Faculty, Endodontics Division at the University of Maryland Dental School Baltimore, Maryland, USA.
Diagnosing Dental and Orofacial Pain: A Clinical Manual approaches a complex topic in a uniquely practical way. This text offers valuable advice on ways to observe and communicate effectively with patients in pain, how to analyze a patients pain descriptions, and how to provide a proper diagnosis of orofacial pain problems that can arise from a myriad of sources anywhere from teeth, joint and muscle pain, and paranasal sinuses to cluster headaches, neuralgias, neuropathic pain and viral infections. Helps the student and practitioner understand the diagnostic process by addressing the exact questions that need to be asked and then analyzing verbal and non-verbal responses to these Edited by experts with decades of clinical and teaching experience, and with contributions from international specialists Companion website provides additional learning materials including videos, case studies and further practical tips for examination and diagnosis Includes numerous color photographs and illustrations throughout to enhance text clarity
Alex J. Moule is an Associate Professor and Discipline Lead in Endodontics at the School of Dentistry, University of Queensland, Brisbane, Queensland, Australia. M. Lamar Hicks is Clinical Professor, Deans Faculty, Endodontics Division at the University of Maryland Dental School Baltimore, Maryland, USA.
Title Page 5
Copyright Page 6
Contents 7
Contributors 8
Acknowledgments 9
About the Companion Website 10
Chapter 1 Introduction 11
Introduction 11
Chapter 2 The Art of Listening – Communicating Effectively with a Patient in Pain 13
Introduction 13
Chapter 3 Causes of Pain in the Orofacial Region 16
Introduction 16
Causes of orofacial pain 17
Dental causes 17
Mucosal causes 17
Pain from temporomandibular disorder (TMD) 17
Masticatory muscle disorders (muscle pain) 17
Temporomandibular joint pain 17
Headaches associated with TMD 18
Referral of pain from neck 18
Paranasal sinus-related orofacial pain 18
Trigeminal nerve pain 19
Facial nerve-related orofacial pain 19
Glossopharyngeal nerve-related orofacial pain 21
Occipital nerve pain 21
Superior laryngeal nerve 21
Salivary gland pain 22
Neurovascular causes of orofacial pain 22
Viral causes of orofacial pain 23
Neuropathic pain 23
Central sensitization 23
Heterotrophic pain 23
Intracranial lesions 23
Psychological aspects of pain experience 24
Genetic factors affecting pain diagnosis 24
Medical conditions that can cause orofacial pain 25
Summary 25
Chapter 4 Gathering Information for an Accurate Pain Diagnosis 26
Introduction 26
Screening questions 26
Basic information gathering 27
What can I do for you (How may I help you)? 27
Historical reporting 28
Self-diagnosing patients 28
Factual reporting 28
Evasive patients 28
Further basic information gathering 28
What do you think is the cause of your pain? 28
Chapter 5 Analyzing Patients in Pain – Describing Pain and the Importance of Descriptors 29
What sort of pain are you having? 29
Severity 29
Descriptors 29
Importance of descriptors in diagnosis of orofacial pain 30
Sensory descriptors 31
Chapter 6 Analyzing Patients in Pain – Observing Patients in Pain 33
Introduction 33
Placing a fingernail vertically between two teeth 35
Moving a fingernail on a tooth 35
Placing a finger over the apex of a tooth 35
Pressing on the gingival margin 36
Rubbing a finger rapidly back and forth across attached gingiva 36
Holding one tooth 36
Holding or moving several teeth 36
Touching the side of the face 37
Pressing under the maxilla 39
Pressing on the body of the mandible with fingers in motion 39
Moving fingers in line under the mandible 39
Describing pain on all lower teeth by running a finger around the gingival margin 40
Describing pain with two hands 40
Bilateral pain 41
Percussion pain on multiple teeth 41
Holding a hand on the side of the face 42
Complaining of inability to sleep on one side of the face 42
Pointing to an area, but reluctant to touch it 42
Complaining of altered sensation 43
Describing pain in and around the eye 43
Describing pain between the eyes 44
Describing pain around the base of the skull 44
Chapter 7 Analyzing Patients in Pain – Associations with Cold and Heat 46
Introduction 46
Temperature sensitivity 46
Pain to cold 46
Bilateral sensitivity to cold 46
Pain to cold relieved by heat 47
Pain to heat 47
Pain to heat relieved by cold 47
A delayed response to heat 47
Unexplained sensitivity to cold on posterior teeth 48
Root-filled teeth sensitive to cold 48
Pain when the patient goes out into the cold 49
Pain to swallowing cold foods or drinks (ice cream headache) 49
Pain relieved by hot pack or hot shower, or by placement of hand on side of face 50
Chapter 8 Analyzing Pain Descriptions – Pain on Biting or Eating and Other Considerations 51
Introduction 51
Pain on biting 51
Pain in vital posterior teeth on biting 52
Biting pain in vital anterior teeth 52
Pain on eating 52
Pain before eating 52
Pain at the commencement of chewing 52
Pain when chewing 53
Pain after eating 53
Pain on biting accompanied by a bad taste 53
Pain relieved by biting 53
Biting pain after a crown is placed on a root canal-filled tooth 53
Other descriptions 54
Pain on swallowing 54
Pain to tongue pressure 54
Pain when traveling on an aircraft, diving or climbing 54
Chapter 9 Analyzing Pain Descriptions –Time Analysis and the Diagnosis of Orofacial Pain 56
Introduction 56
Pain that occurs at a specific time each day 58
Pain on waking in the morning 58
Pain in the afternoon or evening 58
Chapter 10 Analyzing Pain Descriptions – Factors Influencing the Pain 60
Relief of pain 60
Analgesics and pain diagnosis 60
Local anaesthesia and pain diagnosis 61
Antibiotics and pain diagnosis 61
Endodontics and pain diagnosis 61
Chapter 11 Tests and Testing 63
Pulp sensibility (vitality) tests 63
Percussion 65
Palpation 65
Periodontal probing 65
Radiographs 66
Cone beam computed tomography 67
Bite testing 68
Tooth mobility 69
Selective anaesthesia 69
Muscle pain and selective anaesthesia 69
Transillumination 69
Magnification 70
Test cavity 70
Ultrasound 70
Chapter 12 Diagnosing Dental Pain 71
Introduction 71
Clinical progression of pulpal disease 71
Phase 1 72
Phase 2 72
Phase 3 72
Phase 4 72
Phase 5 72
Phase 6 73
Phase 7 73
Phase 8 73
Confirmatory tests for dental pain 73
Treatment considerations 74
Some useful questions if a dental cause is suspected 74
Referral of dental pain 75
Pain is usually referred in a cephalic direction (towards the cranium) 75
Convergence of neurons occurs from same region in the trigeminal spinal nucleus 75
Vertical lamination pattern of representation in the spinal trigeminal 75
Peripheral and central sensitization 75
Most frequently referred pain occurs within a single nerve root 76
Confirmatory tests and findings 77
Questions to ask if referred pain is suspected 77
Chapter 13 Diagnosing Cracked (Crown Fractured) Teeth 78
Cracked (crown fractured) teeth 78
Risk sites 78
Cause of pain 78
Management of cracked teeth 79
1. Tooth identification 79
2. Crack confirmation 79
Direct vision 79
Transillumination 80
Bite testing 82
Selective percussion 82
Controlled wedging and rebound pain 82
Clamp or retainer test 83
Other signs and symptoms of a crack 84
3. Crack investigation 84
4. Treatment planning 85
Type of crack 85
Type of pain 85
Prevention better than a cure 88
Questions to ask when considering a cracked tooth 88
Chapter 14 Diagnosing Joint and Muscle Pains 89
Introduction 89
Masseter 89
Temporalis 89
Digastric 89
Sternocleidomastoid (SCM) 89
Pterygoids 90
Trapezius 90
Temporomandibular disorder 90
Temporomandibular disorders associated with pain 92
Masticatory muscle pain 94
Confirmatory tests for jaw muscle pain 94
Treatment considerations for jaw muscle pain 94
Arthralgia 94
Confirmatory tests for arthralgia 95
Treatment considerations for arthralgia 95
Headaches associated with TMD 95
Diagnosing TMD 95
Intra-articular diagnoses in TMD 96
Confirmation of intra-articular diagnosis (clinical examination) 96
Confirmation of intra-articular diagnosis (imaging) 96
Treatment considerations for TMD 97
Chapter 15 Diagnosing Pain Referral from Neck and Shoulders 99
Pain referral from neck and shoulders 99
Pain referral from muscles 99
Cervicogenic disorders 100
Postural changes 100
Tongue scalloping 100
Elevated hyoid position 100
Temporomandibular disorders (TMDs) 101
Common cervical spine disorders likely to present in a dental setting 101
Cervicalgia 101
Cervical strains and sprains 101
Cervical osteoarthritis 101
Radiculopathy 101
Examination of cervicogenic disorders 102
Posture assessment 102
Treatment considerations 103
Useful questions if pain referral from neck and shoulder is suspected 104
Chapter 16 Diagnosing Pain from the Sinuses 106
Introduction 106
Classification of sinus pain 106
Maxillary sinusitis presenting as toothache or facial pain 106
Maxillary sinusitis of dental origin 107
Confirmatory tests for maxillary sinusitis 110
Treatment considerations 111
Treatment considerations for odontogenic maxillary sinusitis 112
Helpful questions to ask if you suspect a patient has pain from maxillary sinusitis 112
Chapter 17 Diagnosing Tension Headaches and Migraine 113
Introduction 113
Tension-type headache 113
Useful question to ask if tension headache is suspected 114
Confirmatory tests 114
Treatment considerations 114
Migraine headache 114
Useful questions to ask if migraine headache is suspected 115
Confirmatory tests and clinical findings 115
Treatment considerations 115
Chapter 18 Diagnosing Cluster Headaches 116
Introduction 116
Associated autonomic symptoms 116
Prevalence 116
Cause 116
Diagnosis 116
Useful questions to ask if cluster headache is suspected 117
Confirmatory tests 118
Treatment considerations 118
Acute treatment 118
Preventative treatment 118
Chapter 19 Diagnosing Trigeminal Neuralgia 119
Trigeminal neuralgia 119
Cause 119
Diagnosis 119
Other causes 119
Pre-trigeminal neuralgia 119
Glossopharyngeal neuralgia 120
Useful questions to ask if trigeminal neuralgia is suspected 120
Confirmation tests for trigeminal neuralgia (TN) 121
Treatment options 122
Chapter 20 Viruses as a Cause of Orofacial Pain 123
Viral infection as an etiologic source of orofacial pain 123
Varicella zoster virus 123
Orofacial herpes zoster (shingles) 123
Diagnosing facial herpes zoster 124
Useful questions to ask the patient for facial herpes zoster (shingles) of CN V 125
Confirmatory tests for herpes zoster 125
Treatment considerations for herpes zoster 125
Ramsay Hunt syndrome 125
Useful questions to ask if Ramsay Hunt syndrome is suspected 125
Post-herpetic neuralgia 126
Useful questions to ask if 126
Confirmatory tests for orofacial PHN 126
Treatment considerations for orofacial PHN 126
Chapter 21 Vascular Causes of Headaches 127
Giant cell arteritis 127
Headache 127
Systemic symptoms 127
Tenderness 127
Visual disturbances 127
Claudication 127
Localized ischemic complications 128
Questions to ask if giant cell arteritis is suspected 129
Confirmatory tests 130
Treatment considerations 130
Cranial (carotid) artery dissection 130
Questions to ask if cranial nerve dissection is suspected 131
Confirmatory tests 131
Treatment considerations 132
Chapter 22 Diagnosing Neuropathic Orofacial Pain 133
Types of neuropathic orofacial pain 133
Clinical presentation of neuropathic orofacial pain 134
Diagnosing the pain problem 136
Psychosocial and behavioral factors 137
Triggering factors 137
Maintaining factors 137
Management 138
Questions to ask if trigeminal neuropathic facial pain is suspected 138
Presentation and confirmation tests 139
Treatment considerations 139
Reassurance 139
Medication 139
Psychological treatment 139
Chapter 23 Referral Strategies for Orofacial Pain Cases 140
Introduction 140
Coordinating with the general medical practitioner 140
Indications of urgent referral 140
Referral for pain diagnosis and management 141
Useful questions to consider when assessing whether to refer a patient 141
References 143
Index 150
EULA 155
| Erscheint lt. Verlag | 5.12.2016 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Allgemeines / Lexika |
| Medizin / Pharmazie ► Medizinische Fachgebiete | |
| Studium ► 2. Studienabschnitt (Klinik) ► Anamnese / Körperliche Untersuchung | |
| Medizin / Pharmazie ► Zahnmedizin | |
| Schlagworte | Dental Pain • dentistry • Dentistry Special Topics • Endodontics • Endodontie • Endodontik • jaw pain • joint pain • Medical Science • Medizin • Mundheilkunde • muscle pain • Non-Odontogenic Pain • odontogenic pain • Orofacial • Orofacial Pain • Orofaziale Schmerzen • Pain (including Headache) • Schmerzen, Kopfschmerzen • Spezialthemen Zahnmedizin • Tooth Fracture • tooth pain • Zahnmedizin • Zahnschmerz |
| ISBN-10 | 1-118-92499-1 / 1118924991 |
| ISBN-13 | 978-1-118-92499-0 / 9781118924990 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: PDF (Portable Document Format)
Mit einem festen Seitenlayout eignet sich die PDF besonders für Fachbücher mit Spalten, Tabellen und Abbildungen. Eine PDF kann auf fast allen Geräten angezeigt werden, ist aber für kleine Displays (Smartphone, eReader) nur eingeschränkt geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich