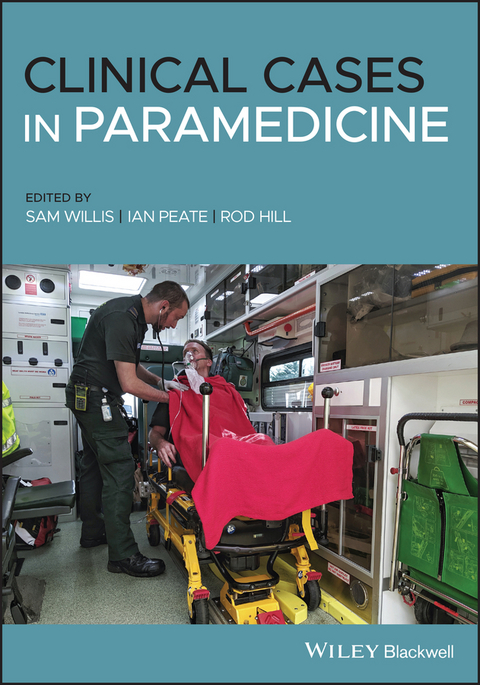
Clinical Cases in Paramedicine (eBook)
John Wiley & Sons (Verlag)
978-1-119-62103-4 (ISBN)
Clinical Cases in Paramedicine provides students, educators, and early career paramedics with a diverse range of detailed case studies that realistically represent the conditions, scenarios, and challenges encountered in practice. Integrating evidence-based cases and expert insights from leading academics and practitioners, this engaging resource helps readers develop appropriate decision-making skills and apply theoretical concepts to practical situations. Organised by medical presentations and body systems, the text provides readers with a systematic framework that mirrors how paramedics assess cases in the real world.
Throughout the text, cases of varying levels of complexity are designed to meet the needs of Case-Based Learning (CBL) and Problem-Based Learning (PBL) curricula used in paramedic training programmes worldwide. Each chapter contains six case studies-introductory, intermediate, and advanced-and features interactive learning activities, discussion questions, practical tips, and authoritative guidance aligned to national and international best-practice standards. Case studies illustrate scenarios related to trauma, medical emergencies, obstetrics, respiratory and cardiac events, minor injuries, drug overdoses, and many others. This comprehensive resource:
- Features case studies of varying lengths and degrees of complexity to suit different readers, from student to professional
- Suitable for use in many international programmes
- Offers chapter introductions and summaries, practice questions, and additional online resources
- Contains clinical, legal, ethical, cultural, remote and rural case studies
- Includes a cumulative and comprehensive 'Test Your Knowledge' concluding chapter
Those studying or working in paramedicine must keep pace with changes in the field using the latest evidence and expert opinion. Clinical Cases in Paramedicine is an essential volume for paramedic students and early-career professionals, as well as educators, lecturers, and trainers.
SAM WILLIS is a Lecturer in Paramedicine at Curtin University and makes contributions to the profession through his innovative teaching practices and publications. He holds a number of professional registrations including as a paramedic and a Teaching Fellow with the UK Higher Education Academy. He is currently undertaking a PhD in the field of Paramedic Education.
IAN PEATE, OBE FRCN, is Head of School, School of Health Studies, Gibraltar, Visiting Professor of Nursing, Northumbria University and St George's University of London, Visiting Senior Clinical Fellow, University of Hertfordshire, Editor-in-Chief of the British Journal of Nursing and Consultant Editor of the Journal of Paramedic Practice.
ROD HILL is Professor of Physiology and Head of the School of Biomedical Sciences at Charles Sturt University. Rod has brought broad impact as a Fellow of the American Association for the Advancement of Science. Rod leads the Charles Sturt paramedicine team which offered the first university programme for paramedicine in Australia in 1995, and is the leading Australian programme in both graduate and undergraduate level paramedicine.
Clinical Cases in Paramedicine provides students, educators, and early career paramedics with a diverse range of detailed case studies that realistically represent the conditions, scenarios, and challenges encountered in practice. Integrating evidence-based cases and expert insights from leading academics and practitioners, this engaging resource helps readers develop appropriate decision-making skills and apply theoretical concepts to practical situations. Organised by medical presentations and body systems, the text provides readers with a systematic framework that mirrors how paramedics assess cases in the real world. Throughout the text, cases of varying levels of complexity are designed to meet the needs of Case-Based Learning (CBL) and Problem-Based Learning (PBL) curricula used in paramedic training programmes worldwide. Each chapter contains six case studies introductory, intermediate, and advanced and features interactive learning activities, discussion questions, practical tips, and authoritative guidance aligned to national and international best-practice standards. Case studies illustrate scenarios related to trauma, medical emergencies, obstetrics, respiratory and cardiac events, minor injuries, drug overdoses, and many others. This comprehensive resource: Features case studies of varying lengths and degrees of complexity to suit different readers, from student to professional Suitable for use in many international programmes Offers chapter introductions and summaries, practice questions, and additional online resources Contains clinical, legal, ethical, cultural, remote and rural case studies Includes a cumulative and comprehensive "e;Test Your Knowledge"e; concluding chapter Those studying or working in paramedicine must keep pace with changes in the field using the latest evidence and expert opinion. Clinical Cases in Paramedicine is an essential volume for paramedic students and early-career professionals, as well as educators, lecturers, and trainers.
SAM WILLIS is a Lecturer in Paramedicine at Curtin University and makes contributions to the profession through his innovative teaching practices and publications. He holds a number of professional registrations including as a paramedic and a Teaching Fellow with the UK Higher Education Academy. He is currently undertaking a PhD in the field of Paramedic Education. IAN PEATE, OBE FRCN, is Head of School, School of Health Studies, Gibraltar, Visiting Professor of Nursing, Northumbria University and St George's University of London, Visiting Senior Clinical Fellow, University of Hertfordshire, Editor-in-Chief of the British Journal of Nursing and Consultant Editor of the Journal of Paramedic Practice. ROD HILL is Professor of Physiology and Head of the School of Biomedical Sciences at Charles Sturt University. Rod has brought broad impact as a Fellow of the American Association for the Advancement of Science. Rod leads the Charles Sturt paramedicine team which offered the first university programme for paramedicine in Australia in 1995, and is the leading Australian programme in both graduate and undergraduate level paramedicine.
Preface vi
List of Contributors vii
Chapter 1 Respiratory emergencies 1
Jennifer Stirling Clare Sutton and Georgina Pickering
Chapter 2 Cardiac emergencies 25
Michael Porter and Joel Beake
Chapter 3 Neurological emergencies 47
Kristina Maximous
Chapter 4 Abdominal emergencies 74
Tania Johnston and Mark Hobson
Chapter 5 Palliative and end-of-life care 99
Alisha Hensby and Samantha Sheridan
Chapter 6 Medical emergencies 118
Tom E. Mallinson
Chapter 7 Non-technical skills 142
Georgette Eaton
Chapter 8 Trauma cases 161
Tom E. Mallinson and Fenella Corrick
Chapter 9 Paediatric cases 186
Erica Ley
Chapter 10 Patient-centred care in complex cases 203
Yasaru Gunaratne and David Krygger
Chapter 11 Legal and ethical cases 225
Ruth Townsend
Chapter 12 Mental health cases 242
David Davis Tom Hewes Lynne Walsh and Brian Mfula
Chapter 13 Older adults 261
Sam Taylor
Chapter 14 Obstetric cases 280
Aimee Yarrington
Chapter 15 Remote area cases 301
Steve Whitfield and Kerryn Wratt
Chapter 16 Mining emergencies 323
Paul Grant and Curtis Northcott
Index 348
Chapter 1
Respiratory emergencies
Jennifer Stirling, Clare Sutton and Georgina Pickering
Charles Sturt University, Bathurst, NSW, Australia
CHAPTER CONTENTS
- Level 1: Asthma
- Level 1: Chronic obstructive pulmonary disease (COPD)
- Level 2: Pulmonary embolism (PE)
- Level 2: Life‐threatening asthma
- Level 3: Respiratory sepsis
- Level 3: Smoke inhalation
LEVEL 1 CASE STUDY
Asthma
| Information type | Data |
| Time of origin | 17:08 |
| Time of dispatch | 17:10 |
| On‐scene time | 17:20 |
| Day of the week | Friday |
| Nearest hospital | 30 minutes |
| Nearest backup | 15 minutes |
| Patient details | Name: Betsy Booper DOB:10/09/2002 |
CASE
You have been called to an outdoor running track for an 18‐year‐old female with shortness of breath. The caller states she has taken her inhaler to no effect.
Pre‐arrival information
The patient is conscious and breathing. You can access the area via the back gate of the sports field and drive right up to the patient, who is sat down on the track.
Windscreen report
The location appears safe. Approx. 10 people around the patient. Environment – warm summer evening and good light.
Entering the location
The sports coach greets you as you get out of the ambulance and informs you that the patient suffers with exercise‐induced asthma, but this is worse than normal and her inhaler has been ineffective.
On arrival with the patient
The patient is sat on a bench on the side of the track. She is leaning forward, resting her elbows on her thighs (tripodding). She says hello as you introduce yourself to her.
Patient assessment triangle
General appearance
Alert. Speaking in short sentences. She looks panicked.
Circulation to the skin
Flushed cheeks.
Work of breathing
Breathing appears rapid and shallow. An audible wheeze is noted.
SYSTEMATIC APPROACH
Danger
None at this time.
Response
Alert on the AVPU scale.
Airway
Clear.
Breathing
RR: 28. Regular and shallow. No accessory muscle use. Expiratory wheeze on auscultation.
Circulation
HR: 100. Regular and strong. Capillary refill time <2 seconds. Flushed cheeks and peripherally warm.
Disability
Moving all four limbs.
Pupils equal and reactive to light (PEARL).
Exposure
Bystanders have left. Next of kin are now on scene.
Temperature: warm summer evening – approx. 20 °C.
Vital signs
RR: 28 bpm
HR: 100 bpm
BP: 125/74 mmHg
SpO2: 93%
Blood glucose: 5.2 mmol/L
Temperature: 36.9 °C
PEF: 300 L/min
GCS: 15/15
4 Lead ECG: sinus tachycardia
TASK
Look through the information provided in this case study and highlight all of the information that might concern you as a paramedic.
- Aside from auscultation, which you have already done, what examination techniques should you incorporate into this patient assessment?
- Inspection – observe the chest for an abnormalities such as wounds, scars, bruising, asymmetry and recession.
- Palpation – feel for any asymmetry, vocal fremitus and tenderness.
- Percussion – hyper‐ or hypo‐resonance.
- What adventitious (added) sounds might indicate asthma and why?
Expiratory wheeze. This sound is made when air has a restricted path through the bronchi, due to inflammation and muscle spasm in the airways.
- What medicine (pharmacology) is likely to relieve the patient’s symptoms and why?
Nebulised salbutamol – it is a Beta2, adrenergic agonist that relaxes smooth muscle in the bronchi.
Case Progression
You treat the patient with 5 mg of nebulised salbutamol and 6 L of oxygen. The nebuliser finishes and you remove the mask.
Patient assessment triangle
General appearance
The patient is now speaking in full sentences.
Circulation to the skin
Flushed.
Work of breathing
Normal effort of breathing.
SYSTEMATIC APPROACH
Danger
None at this time.
Response
Alert.
Airway
Clear.
Breathing
RR:16. Regular. Normal depth. No accessory muscle use. No wheeze or adventitious sounds.
Circulation
HR: 105. Regular and strong. Capillary refill time <2 seconds. Flushed cheeks and peripherally warm.
Disability
No change.
Exposure
No change.
Vital signs
RR: 16 bpm
HR: 105 bpm
BP: 128/78 mmHg
SpO2: 97%
Blood glucose: not repeated
Temperature: not repeated
PEF: 380 L/min
GCS: 15/15
4 lead ECG: sinus tachycardia
- What kinds of questions would you ask this patient specifically related to asthma as part of the history‐taking process?
See Table 1.1.
Table 1.1 History‐taking questions
| Asthma history Does this feel like your normal asthma? Is this the worst it’s ever been? What time did this episode start today? Do you take your asthma medication regularly? What were you doing when it started today? What usually triggers your symptoms? When was the last time your visited your GP and/or went to hospital with these symptoms? Have you ever been intubated or been in ICU with these symptoms? Medication history What asthma medications do you take? How frequently do you have to take your medication? Do you usually have to take your inhaler while exercising? When was the last time you had a medication review with your GP? Have you had any recent changes in medication? Do you take any other medications? Have you had any coaching on the best way to take your inhaler? F/SH (family and social history) Does anyone else in your family experience asthma? Do you smoke? If so, how frequently? Do you drink or take any drugs recreationally? Who do you live with? What do you do for work? Do you exercise regularly? Are you under any particular stress at the moment? Past medical history (PMH) Do you have any other medical problems? Do you have any allergies? Have you had a cough or cold recently? |
- The patient is 160 cm tall, what should her predicted peak expiratory flow reading (PEFR) be? Her first reading was 300 – what percentage is that from predicted?
(Hint: you will be required to look this up using the Australian National Asthma Council chart found here: http://www.peakflow.com/pefr_normal_values.pdf or by doing an internet search.)
- 400 L/min.
- 75%.
LEVEL 1 CASE STUDY
Chronic obstructive pulmonary disease (COPD)
| Information type | Data |
| Time of origin | 07:09 |
| Time of dispatch | 07:12 |
| On‐scene time | 07:30 |
| Day of the week | Wednesday |
| Nearest hospital | 15 minutes |
| Nearest backup | 40 minutes |
| Patient details | Name: Dave Beater DOB: 21/09/1954 |
CASE
You have been called to a residential address for a 66‐year‐old male with difficulty in breathing. The caller states he has been breathless all night and has had a cough recently. He has seen his GP who prescribed antibiotics and steroids but he feels his breathing has got worse overnight.
Pre‐arrival information
The patient is conscious and breathing and is in a first‐floor...
| Erscheint lt. Verlag | 25.2.2021 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Allgemeines / Lexika |
| Medizin / Pharmazie ► Gesundheitsfachberufe | |
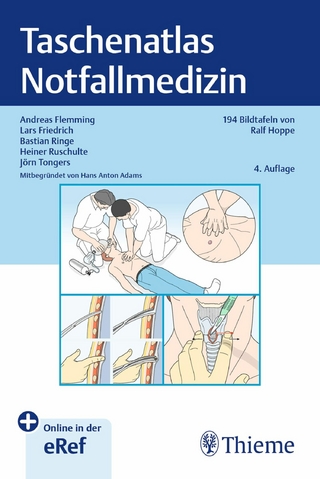
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Notfallmedizin | |
| Medizin / Pharmazie ► Pflege | |
| Sozialwissenschaften ► Soziologie | |
| Schlagworte | Acute, Critical & Emergency Care • Emergency Medicine & Trauma • Intensive/Critical Care • Intensivpflege • Intensiv- u. Notfallpflege • Krankenpflege • Medical Science • Medizin • Notfallmedizin • Notfallmedizin u. Traumatologie • nursing • paramedic cases • paramedic case studies • paramedicine case-based learning • paramedicine cases • paramedicine case studies • paramedicine curricula • paramedicine problem-based learning • paramedicine problems • paramedicine training • paramedic training |
| ISBN-10 | 1-119-62103-8 / 1119621038 |
| ISBN-13 | 978-1-119-62103-4 / 9781119621034 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich