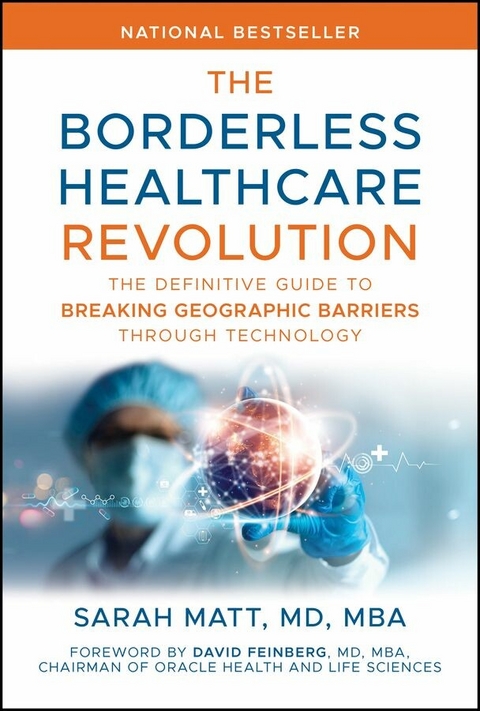
The Borderless Healthcare Revolution (eBook)
458 Seiten
Wiley (Verlag)
978-1-394-35713-0 (ISBN)
Concrete, hands-on strategies for making healthcare more accessible for everyone
The Borderless Healthcare Revolution: The Definitive Guide to Breaking Geographic Barriers Through Technology is your field guide to a future in which a clinic visit is never farther away than the nearest screen and a surgeon's skill can cross oceans in real time. Drawing on two decades at the intersection of medicine and technology. including years as a senior leader at Oracle's global health division, Dr Sarah Matt translates frontier-grade innovation into day-to-day practice for clinicians, health-system strategists, and policymakers who refuse to accept geography as destiny.
Inside you will find concrete playbooks rather than platitudes; every framework has been piloted in settings that range from Manhattan cath labs to Kenyan community clinics. You will also meet the patients and providers whose lived stories prove that digital transformation works only when it works for everyone.
What you will learn:
- The tech that already moves care without moving patients, telemedicine, remote surgery, ambient AI, and how adoption curves exploded after 2020, with more than three quarters of US hospitals now running telehealth programs
- Human-centered design tactics that translate pixels into trust, from inclusive language pivots to offline-first apps that respect bandwidth deserts
- A five-pillar access audit that flags physical, financial, cultural, digital, and trust barriers in any market, plus scorecards to track progress
- Strategy checklists forged during Dr Matt's tenure at Oracle for aligning payers, regulators, and vendors around sustainable reimbursement models
- Future-readiness briefs on robotics and mixed-reality training at a moment when the surgical robotics market is projected to triple by 2031
SARAH MATT, MD, MBA, is a surgeon turned health technology strategist, author, and speaker. She has held leadership roles at Oracle, Sovato, NextGen, and multiple health tech startups, bringing over two decades of experience at the intersection of medicine and innovation. Her work focuses on leveraging digital tools to expand access and reimagine healthcare delivery worldwide.
Concrete, hands-on strategies for making healthcare more accessible for everyone The Borderless Healthcare Revolution: The Definitive Guide to Breaking Geographic Barriers Through Technology is your field guide to a future in which a clinic visit is never farther away than the nearest screen and a surgeon s skill can cross oceans in real time. Drawing on two decades at the intersection of medicine and technology. including years as a senior leader at Oracle s global health division, Dr Sarah Matt translates frontier-grade innovation into day-to-day practice for clinicians, health-system strategists, and policymakers who refuse to accept geography as destiny. Inside you will find concrete playbooks rather than platitudes; every framework has been piloted in settings that range from Manhattan cath labs to Kenyan community clinics. You will also meet the patients and providers whose lived stories prove that digital transformation works only when it works for everyone. What you will learn: The tech that already moves care without moving patients, telemedicine, remote surgery, ambient AI, and how adoption curves exploded after 2020, with more than three quarters of US hospitals now running telehealth programs Human-centered design tactics that translate pixels into trust, from inclusive language pivots to offline-first apps that respect bandwidth deserts A five-pillar access audit that flags physical, financial, cultural, digital, and trust barriers in any market, plus scorecards to track progress Strategy checklists forged during Dr Matt s tenure at Oracle for aligning payers, regulators, and vendors around sustainable reimbursement models Future-readiness briefs on robotics and mixed-reality training at a moment when the surgical robotics market is projected to triple by 2031 Whether you lead a rural health network, build digital products, or craft policy, The Borderless Healthcare Revolution: The Definitive Guide to Breaking Geographic Barriers Through Technology gives you the tools to expand access today and blueprint the borderless systems of tomorrow. Read it; then use it to deliver care that travels at the speed of need.
CHAPTER 1
The Geography Problem
From the Front Lines
The summer heat in Texas hits you like a wall when you step outside. On this particular August morning in 2012, I was making my way up the cracked concrete path to Maria’s mobile home, my medical bag feeling heavier with each step. The window-mounted air conditioning unit hummed desperately against the rising temperature. This was my third attempt to see Maria; we had previously been unable to find her trailer after two attempts to work through an interpreter, poor phone connections, and constantly changing locations of residence. So here I was, bringing the clinic to her. Maria’s story would become one of countless examples I’d encounter of how geography shapes health in ways both obvious and subtle. But let me back up a bit. Let me tell you how I found myself making house calls in the Texas heat, and what it taught me about the deep divide in American healthcare.
When I moved to Austin, TX, I was amazed at the availability of jalapeños. You could literally get them at any restaurant. What’s better than jalapeños? Well, tacos for breakfast, lunch, and dinner of course! The city was bustling with music, people, and cutting-edge tech. It was a far cry from Upstate NY where I grew up. At the same time, the stark contrast within the city nearly gave me whiplash. By night, I navigated the sleek corridors of the UT McCombs MBA program, surrounded by future tech executives and management consultants. These were people of privilege, who were funding advanced degrees, with many of us already managing teams at big firms around town.
But by day, I wound through neighborhoods where the American Dream felt more like a distant mirage, and where few who did not live there would venture. I was providing medical care to patients who couldn’t leave their homes. Patients who nobody wanted to see in their offices, because they were so complex, and whose situations were seemingly unfixable. The city’s famous breakfast tacos and vibrant music scene had drawn me here, but it was these house calls that would reshape my understanding of American healthcare. Each doorway I stepped through told a different story of how geography, whether measured in miles or mere city blocks, could become an insurmountable barrier to care.
Fact Check
- In 2022, 7.8 percent of U.S. counties did not have a primary care physician. The national ratio of primary care physicians was 83.8 per 100,000 people.1
- Over the course of the last 10 years, more than 120 rural hospitals have ceased operations, further limiting access to care for populations which are older, less healthy, and less affluent than their urban counterparts.2
- An analysis of 2021 Medicare claims showed that beneficiaries in rural areas received less specialty care than those in urban areas.3
The Reality of Home-Based Care
So, what does “homebound” actually mean? According to Medicare guidelines, homebound patients have conditions that make leaving home difficult without considerable effort and assistance. When I started practicing in the early 2000s, this meant I could see patients monthly; a stark contrast to the typical once- or twice-yearly primary care visits many Americans experience. This increased frequency of care should have meant better outcomes, but the reality was far more complex.
According to the Centers for Medicare & Medicaid Services (CMS), a patient is considered homebound if they meet the following criteria.4
Criterion One
- The patient must either:
- Require the aid of supportive devices such as crutches, canes, wheelchairs, or walkers; the use of special transportation; or the assistance of another person to leave their place of residence due to illness or injury; or
- Have a condition such that leaving home is medically contraindicated.
Criterion Two
- There must exist a normal inability to leave home; and
- Leaving home must require a considerable and taxing effort.
Even if the patient leaves the home, they may still be considered homebound if the absences are infrequent, of short duration, or for the purpose of receiving healthcare treatment.4
Stories from the Field: Physical Barrier Spotlight
The cards were still scattered across Fred’s small table when we arrived, evidence of the game we’d interrupted. The air in his apartment was thick with the kind of stillness that comes from windows rarely opened. “¿Cómo está?” my medical assistant Art asked, his casual Spanish immediately putting Fred at ease. None of us could have known then how the next few hours would unfold, or that this routine visit would become a race against time.
Fred (Frederico per his chart) was a 66-year-old Spanish speaking Latino man living alone in a 65 and up low-income housing apartment on the southeast side of Austin. Two million elderly Medicare patients were completely or mostly homebound in 2011.5 Fred was just one of this ever-increasing population.
He told me he had “bad feet” for over a decade and scooched along the halls of his apartment complex in a wheelchair at a steady but snail’s pace. He was jovial and when we got to his apartment, he had a friend over playing cards. After his wife died almost five years earlier, he had turned to smoking cigars, didn’t go to the doctor, and had very few ties with his family. But he had a few friends on his floor in the apartment building and generally seemed to be in a good mood. His social worker had referred him to us. She had helped him get on Medicare, get food stamps, and connect him with a free community service to bring him groceries to his apartment. His home was small and cluttered, not particularly well kept, but then again, he was a bachelor doing his best on his own. These stories from Austin aren’t unique to Texas or even to the United States. Across the globe, healthcare systems struggle with similar challenges of access—quality and inclusive care—although their solutions often differ dramatically.
Sometimes I would see new patients without much history to go on, and sometimes it was going to just be a surprise. Less than one-third of primary care physicians in the United States report making home visits, a rate significantly lower than in other high-income countries.6 This time all we knew was that he had “bad feet.” So, when we arrived, we were pretty much ready for anything. My medical assistant fortunately came with me everywhere I went. His Spanish was casual but was extremely helpful when seeing patients. While he had been scolded by more than one abuela for his casual grammar, it was certainly better than my own Spanish, which was abysmal.
We went back and forth with Fred, asking him questions about his living situation, his health history, and any medical problems he might have. He was worried about his feet; they had caused him pain for years and recently they had become even more numb in spots and were “making his socks dirty.” But he said he had no other medical issues, was not on any medications, and had not seen a doctor for many years. So, we drew some blood, and I started my exam. He had a low fever to start, his blood pressure was elevated, and his heart rate was increased. But then again, having a doctor in a white coat at their house often stresses folks out a bit. As I moved through my exam, things continued to be rather insignificant.
Then I asked him to remove his socks and shoes for me so I could look at his legs and feet. He said he couldn’t do it by himself and admitted that he had been wearing this same set of shoes and socks continuously for over a week straight. We removed the shoes, and a terrible stench filled the room. The socks were stuck onto his feet in multiple places, and after removal, revealed multiple wounds, ice cold toes, and no palpable pulses. But what sealed the deal was the redness spreading up his ankle, and a crackling feeling up his leg with discoloration consistent with necrotizing fasciitis. This is “flesh eating bacteria” for the uninitiated. This is a medical emergency. He had not seen the color and crackling feeling a week earlier when he had gotten help to change his socks. In fact, he hadn’t been concerned, because he couldn’t feel it. Approximately 5 percent of U.S. adults report forgoing healthcare due to transportation barriers, with higher percentages among Black adults (8%), individuals with low family incomes (14%), and those with public health insurance (12%).7 Fred couldn’t remember the last time he’d been to the doctor, so it was unclear how long his feet had been going downhill.
Once you have seen necrotizing fasciitis (or smelled it!), you never forget it, and this was textbook. It reminded me of cases I had seen during my surgery training. I was convinced of my diagnosis, and this was an emergency. He needed to go to the ER for a surgical consult immediately. I wanted to call 911 and get him seen right away, but he was hesitant. He couldn’t pay for an ambulance. He couldn’t pay for medications or the copay. He had no one to care for him. His feet had been “bad” for years and he had never had an emergent problem. Plus, we just met. How could I help this man?
Fred was one of my most memorable patients, but this is what I saw day in and day out. Much of the time I did more social work than medicine and did what I could to help...
| Erscheint lt. Verlag | 19.11.2025 |
|---|---|
| Vorwort | David Feinberg |
| Sprache | englisch |
| Themenwelt | Sachbuch/Ratgeber ► Natur / Technik |
| Medizin / Pharmazie ► Medizinische Fachgebiete | |
| Schlagworte | Access to healthcare • Digital Health • Digital Healthcare • healthcare access • Healthcare Robotics • Healthcare Transformation • Rural Healthcare • Smart Healthcare • telemedicine • Virtual healthcare • virtual medicine |
| ISBN-10 | 1-394-35713-3 / 1394357133 |
| ISBN-13 | 978-1-394-35713-0 / 9781394357130 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich