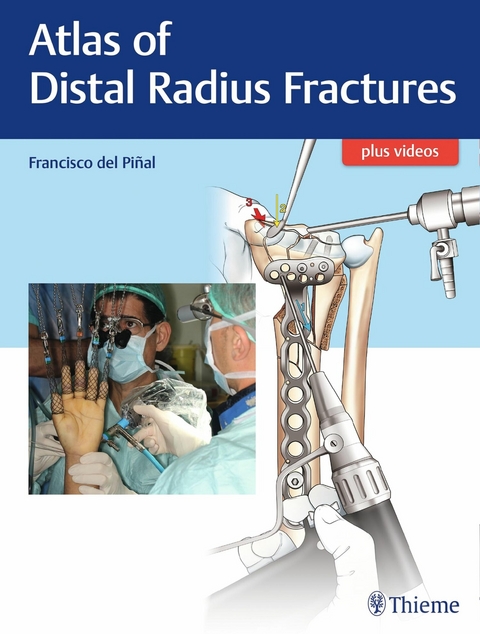
Atlas of Distal Radius Fractures (eBook)
Thieme Medical Publishers (Verlag)
978-1-63853-561-4 (ISBN)
Written by one of the world's foremost authorities, this beautifully illustrated surgical atlas is a case-based presentation of the management of distal radius fractures. Each chapter offers a comprehensive guide to the diagnosis and treatment of a specific fracture, including possible complications and how to prevent them, using detailed photographs and illustrations. The cases are accompanied by high-quality operative video to complete the surgical picture. Special emphasis throughout focuses on avoiding pitfalls and using special techniques to optimize outcomes.Key HighlightsNearly 700 illustrations and intraoperative photographs guide the reader through procedures.Operative video for all chapters, narrated by the author, including detailed explanations and rationale for each maneuver.A focus on the "e;how"e; of surgical technique (rather than the "e;why"e;) keeps attention on the necessary steps, tools, and procedures to address a specific type of fracture.Real cases, presented from beginning to end, cover all of the difficult aspects of fracture management.Francisco del Piñal is considered to be among the world's best hand surgeons. His contributions in arthroscopic surgery techniques for wrist fractures are endorsed and used internationally. This book, written for hand surgeons, orthopaedic surgeons, and plastic surgeons, provides essential insight to specialists and subspecialists alike.
| Prolegomena: Some Initial Thoughts and Facts | 1 |
Fig. 1.1 In this Atlas I am going to skip obvious remarks about distal radius fractures such as it being one of the most common, as this is of very little help when operating our patient. Also I am not going to discuss indications (as they vary from country, practice and patient). This is a surgical atlas and the aim of this book is to show how you can achieve good reproducible results in difficult fractures as the one above. For this purpose, classic knowledge, arthroscopy and, at times, microsurgery are required. The patient shown sustained a fall from a two-story scaffold when he was 18 years old. He was in his first employment.
Fig. 1.2 In a small town, like where I used to work, you meet patients in the street (for the good and the bad), and I knew he was doing very well. About 10 years later I saw him working while I was in a building opposite him. I yelled at him “Haven’t you learned? You should fasten your security belt to the scaffolding,” and he smiled, answering, “I am not afraid knowing you are nearby.” (Incorrigible!) He is now the owner of the company and I am certain he makes everybody comply with the safety measures.
Fig. 1.3 I am also not going to discuss in this Atlas any of the available classifications—Melone, Diego Fernandez, Universal, AO, or the more recent Bain, who has found vulnerable spots for fractures in areas free of ligament insertions. The reason for this is, as you can see on the right, even simple fractures (two-part fractures) can have such a variety of configurations, all of which need to be tackled by different routes and methods. Therefore, although they belong to the same “group,” they share no useful characteristics to aid at surgical planning (akin to grouping pears and apples). However, I do think all classifications are useful. I have learned them all and recommend you memorize them by heart. There is an enormous amount of information behind each of the sketches, and the expertise of giants in the field. They have helped me enormously to understand fracture configurations and patterns of displacement. (Courtesy Dr. Gregory Bain.)
Fig. 1.4 Thus, although I have studied all the classifications and recommend doing so, I rely on good radiographs and computed tomography (CT) for my own practice. From the radiographs I get a general overview of the fracture, and from the CT, I get the detail. From these I gather the information about the fracture configuration and become aware if the fracture has any of the five determinants that, in my experience, make treatment more difficult and give a grimmer prognosis if not tackled correctly. They include the following: (1) multifragmentation of the joint; (2) rim fractures; (3) metaphyseal comminution; (4) free osteochondral fragments; and—last but not least—(5) concomitant ulnar head fracture. Each issue will have its own chapter devoted to it, and will set a higher degree of difficulty for the surgeon—and much more so when combined. Nevertheless, the patient can still achieve a good result. In this case, not only is the fracture complex, but the patient also had a soft tissue defect.
Fig. 1.5 If there is suspicion of articular involvement, then I think it is paramount to have a CT scan. Some people find the CT scan worthless. I think this is so because crude CT images are indeed quite often useless. However, the information one can gather from a properly “worked” CT scan is unsurpassed by any other test. Furthermore, the information is valuable for treatment. To illustrate this, I am going to show how DICOM images can be worked in a program called OsiriX, which is available free online.
The original DICOM images are necessary. They should be approximately 300 to 400 slices per study, and generally they are provided in a soft tissue window.
The choice of images should be changed to “Bone” in the menu (the tab circled in red), and then 3D MPR should be chosen. This will give you the axis and views from three different planes (see Video 1.1). (Courtesy OsiriX, Bernex, Switzerland.)
Fig. 1.6 By using the tabs circled, rotate the images to align them to the anatomic position, rotate the axis, and zoom in as required. (Courtesy OsiriX, Bernex, Switzerland.)
Fig. 1.7 Now not only do you have the axial slices, but also sagittal and coronal slices are visible at exactly the right angles. But this is far from the full information that you need. (Courtesy OsiriX, Bernex, Switzerland.)
Fig. 1.8 By double-clicking on each of the cuts you will have a full screen size of each plane (in this example, the sagittal). By scrolling on the image you will have all the cuts in that plane. Do the same for the coronal and axial planes in order to have a better idea of the fracture configuration. (Courtesy OsiriX, Bernex, Switzerland.)
Fig. 1.9 At a minimum I study five sagittal slices, and I have by convention named them from radial to ulnar S1 to S5: S1, near the styloid; S2, on the middle of the scaphoid fossa; S3, on the sagittal crest; S4, on the middle of the lunate facet; and S5, on the ulnar border of the lunate facet.
Fig. 1.10 Similarly, I also study four cuts in the coronal plane (C1–4, volar to dorsal, evenly distributed) and three in the axial plane (distal to proximal). This set of figures gives a general idea of the fracture and helps to locate step-offs and/or malaligned fragments. Nevertheless, some more work needs to be done to get the maximum from the crude images that the CT scan gives.
Fig. 1.11 The first refined information comes from what I term pure articular view. This is a general overview of the articular surface (like a bird’s-eye view) and is very helpful for the arthroscopy. The general overview is obtained by tilting the axis in the coronal and then in the sagittal images; the joint surface will come into view in the axial angle. (Courtesy OsiriX, Bernex, Switzerland.)
Fig. 1.12 By double-clicking on the articular view, you will have an enlarged image. The exact articular configuration of the fracture can now be studied.
Fig. 1.13 In very displaced fractures or in cases of free osteochondral fragments, it is not possible to garner all the information from a single articular view. However, every fragment can be studied. This image is of a multifragmented fracture with a free osteochondral fragment (arrows) (see Chapter 15).
Fig. 1.14 By centering the axis on the area one wants to study and tilting it to the fragment, the so-called fragment view is obtained. The program has measuring tools that will give an accurate size of the fragment.
Fig. 1.15 I cannot conclude the imaging part without saying that three-dimensional image reconstructions, so loved by radiologists and the lay public alike, are useless for the surgeon. These reconstructed images lack the proper definition to provide the necessary detailed information regarding the fracture fragments. Furthermore, due to software inaccuracy, they often amalgamate fragments that are actually separated.
Fig. 1.16 Regarding fixation, I currently manage most fractures with fixed-angle volar plates. Jorge Orbay bears the honor of having designed the first fixed-angle plate whose distal screws adapted to the curvature of the distal radius (pictured here is the original DVR plate). I may share some DNA with my good friend Jorge, as our families have lived for centuries just 100 km from each other, but we share nothing else.
Fig. 1.17 Unlike classic fixation with plates, in which purchase on the far cortex (circles) is key to the rigidity of the fixation, fixed-angle plates work by creating an internal framework that supports the subchondral plate. The distal row of screws provides support in the center, and the proximal row of screws act more dorsally. By definition the screws should not purchase on the dorsal cortex, but should be 2 mm shorter in order to avoid tendon irritation.
Fig. 1.18 I do not want to expend too much time discussing plates, but I have to make some remarks that are not clearly presented in the literature and that have a high impact on the outcome. Since the first plate was marketed, myriad others have been presented based on the same principle. Despite the fact that all plates available are fixed-angle, they are quite different (and I have learned this the hard way). Some designs do not adapt to the tilt the radius has in the frontal plane: They provide good support in...
| Erscheint lt. Verlag | 5.9.2018 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizinische Fachgebiete ► Chirurgie ► Ästhetische und Plastische Chirurgie |
| Medizinische Fachgebiete ► Chirurgie ► Unfallchirurgie / Orthopädie | |
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Orthopädie | |
| Schlagworte | Distal radius fracture • distal radius fractures • distal radius injury • dry arthroscopy • external fixation • fracture salvages • hand surgery • internal fixation • ligamentous instabilities • Malunions • radial styloid fracture • shoehorn maneuver • ulnar fractures • Wrist arthroscopy |
| ISBN-10 | 1-63853-561-2 / 1638535612 |
| ISBN-13 | 978-1-63853-561-4 / 9781638535614 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
DRM: Digitales Wasserzeichen
Dieses eBook enthält ein digitales Wasserzeichen und ist damit für Sie personalisiert. Bei einer missbräuchlichen Weitergabe des eBooks an Dritte ist eine Rückverfolgung an die Quelle möglich.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich