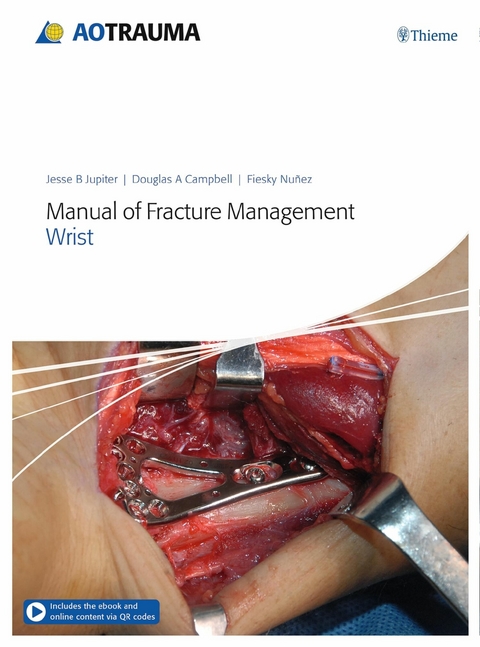
Manual of Fracture Management - Wrist (eBook)
524 Seiten
Thieme (Verlag)
978-3-13-258268-2 (ISBN)
2 Carpals
2.1 Scaphoid—nondisplaced fracture treated percutaneously with a headless compression screw
1 Case description
Fig 2.1-1a–b A 26-year-old man fell onto his outstretched right hand during a club soccer game noting immediate acute pain. An examination revealed pain in the anatomical snuff box of his wrist. The AP and lateral x-rays revealed a fracture line across the waist of the scaphoid, however, carpal alignment appeared normal.
Fig 2.1-2a–c The 2-D and 3-D CT scans identified the fracture as having minimal displacement but going through both cortices of the scaphoid in the frontal and sagittal planes (arrows).
2 Indications
Nondisplaced scaphoid fractures
Fig 2.1-3 Percutaneous (minimally invasive) fixation is largely indicated for nondisplaced or minimally displaced fractures of the waist of the scaphoid.
Internal fixation vs nonoperative treatment
In general, internal fixation of fractures is thought to provide effective bone healing in at least the same if not less time than nonoperative treatment, but that the period of immobilization is shortened. Percutaneous treatment brings the advantages of avoiding a wide surgical approach, preserving the palmar ligament complex and local vascularity, and avoiding the extended immobilization required for healing after a wider open exposure.
Readers of this publication are immediately reminded that in some instances of wrist injury, nonoperative treatment is a viable alternative. However, the detailed cases provided throughout this book outline situations where, for those patients, surgical techniques were deemed the more appropriate treatment option.
Imaging
With nondisplaced and minimally displaced scaphoid fractures, conventional x-rays often do not adequately demonstrate the complete fracture configuration. As shown in the case description of this patient, CT scans were therefore performed and are strongly recommended if a percutaneous procedure is planned.
Anatomical considerations
Fig 2.1-4a–e With all scaphoid fractures, the anatomy and vascularity of the scaphoid need to be considered. Close to 80% of the surface of the scaphoid is covered with articular cartilage, which greatly limits the points of entry for fixation devices. An additional constraint is the curved morphology of the scaphoid. This means that it can be difficult to pass a wire or fixation device along the true long axis of the bone, yet this is the implant location that provides the greatest stability and compression. Occasionally, access to the correct distal entry point for a device can only be gained by a limited excision of the overhanging edge of the trapezium.
Vascularity
Fig 2.1-5a–b The blood supply of the scaphoid is derived from two sources. The main source is a group of blood vessels entering the dorsal surface of the distal pole (a). This is the largest contribution to the vascularity of the scaphoid as the dorsal group supplies the proximal two thirds of the bone. However, the proximal pole relies on a retrograde blood flow, a fact that makes this part of the scaphoid more prone to suffer avascular bone necrosis and a consequent nonunion.
A second group of vessels enters the palmar aspect of the distal pole (b). These vessels contribute largely to the vascularity of the distal third.
3 Preoperative planning
Equipment
• Headless compression screw set 2.4 or 3.0
• 1.1 mm K-wires, 150 mm length
• Hypodermic needle
• Osteotome
• Image intensifier
Patient preparation and positioning
Fig 2.1-6 Before starting the procedure, re-examine the fracture pattern under an image intensifier. Be sure that the fracture is suitable for a percutaneous technique and that no secondary displacement has occurred. Position the patient supine and place the forearm on the hand table. By abducting the patient’s shoulder it is possible for the surgeon and the assistant to sit on either side of the hand table. A nonsterile pneumatic tourniquet is used. Prophylactic antibiotics are optional.
4 Surgical approach
Approach
Fig 2.1-7a–b Two approaches exist for percutaneous screw fixation, entering either palmarly (a) or dorsally (b) to reach the scaphoid from either the distal or proximal pole. For the patient in this chapter, the palmar approach was used, entering through the distal pole of the scaphoid.
Hyperextend the wrist
Fig 2.1-8 To assist in the approach, place a rolled towel or bolster under the wrist and hyperextend it. The use of the support helps access the correct entry point for a guide wire.
Mark the skin
Fig 2.1-9 It can be helpful to mark on the skin the position of the scaphoid, the palmar rim of the distal radius, and the level of the scaphotrapezial joint.
Skin incision
A stab incision of 5–10 mm is made distally to the scaphotrapezial joint. Deepen the incision through the subcutaneous tissues by blunt dissection then incise the capsule of the scaphotrapezial joint. The distal pole of the scaphoid is now accessible for insertion of a K-wire, which will be used as a guide wire.
5 Reduction
Determine insertion point for the guide wire
Fig 2.1-10a–b The correct entry point for the guide wire is the center of the distal pole of the scaphoid. However, to get proper access, it may be necessary to remove the palmar ridge of the trapezium with an osteotome or a bone nibbler/rongeur. This reveals the distal pole of the scaphoid and allows the path of the guide wire to be made more centrally within the bone.
Fig 2.1-11a–b Use a hypodermic needle to determine the insertion point radiologically before inserting the guide wire.
Insert the guide wire
Fig 2.1-12a–c The guide wire should be inserted through a drill guide (a). If no drill guide is available, use a protective sleeve. The position of the wire should be as perpendicular as possible to the fracture line (b–c). In oblique fractures, this principle may have to be compromised. Do not penetrate beyond the proximal cortex of the scaphoid.
Fig 2.1-13a–c The guide wire was inserted at the confirmed entry point.
6 Fixation
Measure screw length
Fig 2.1-14a–b Two methods can be employed for measuring the desired length of the headless screw. Insert the dedicated measuring device over the guide wire, through the drill guide, which must be firmly positioned on the tubercle for a reliable measurement (a). Alternatively, if the dedicated measuring device is not available, take another guide wire of the same length and place its tip onto the bone at the insertion point (b). The difference between the protruding ends of the two wires indicates the length of the drill hole for the screw. Subtract 2–3 mm to determine the screw length.
Drilling
Fig 2.1-15 Use only the dedicated drill bit. A power drill will exert less force on the fragments than manual drilling and will reduce the risk of displacing the fragments. A small power drill with slow rotation is the preferred choice. Use saline solution to cool the drill bit in order to minimize thermal injury. Check the position of the tip of the drill bit under image intensification.
Select the screw
Fig 2.1-16a–d Select the appropriately sized cannulated (ie, hollow) headless compression screw (a–c). The selected screw is inserted into the internal thread of the compression sleeve (d).
Insert the screw
Fig 2.1-17 The screw and compression sleeve are inserted over the guide wire.
Fig 2.1-18a–c The screw is tightened until sufficient compression is achieved.
Fig 2.1-19a–b The cannulated screwdriver is inserted. The compression sleeve is held still, using the thumb and index finger to firmly hold the compression sleeve, as the screwdriver turns the screw and advances it out of the compression sleeve and into the bone. Compression is maintained by the compression sleeve during this action.
Advance and countersink the screw
Fig 2.1-20a–c The screwdriver has three colored markings that are visible at the edge of the compression sleeve. The green mark indicates the screw is still fully retained within the compression sleeve (a). The yellow mark...
| Erscheint lt. Verlag | 25.4.2019 |
|---|---|
| Verlagsort | Stuttgart |
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Medizinische Fachgebiete ► Orthopädie |
| Schlagworte | fracture and injury types • Malunions • Nonunions • Osteoarthritis • Postoperative Complications |
| ISBN-10 | 3-13-258268-9 / 3132582689 |
| ISBN-13 | 978-3-13-258268-2 / 9783132582682 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
DRM: Digitales Wasserzeichen
Dieses eBook enthält ein digitales Wasserzeichen und ist damit für Sie personalisiert. Bei einer missbräuchlichen Weitergabe des eBooks an Dritte ist eine Rückverfolgung an die Quelle möglich.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich