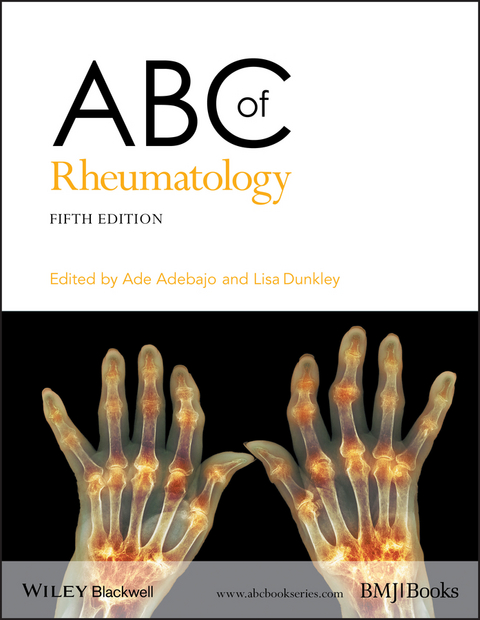
ABC of Rheumatology (eBook)
John Wiley & Sons (Verlag)
978-1-118-79318-3 (ISBN)
ABC of Rheumatology continues to be a practical and informative guide to the assessment, treatment and management of common rheumatic and musculoskeletal conditions within primary care.
Fully updated to reflect developments in this fast growing field, the fifth edition covers overviews of all key areas of rheumatology, and includes new chapters on radiology and immunology, as well as expanded coverage on metabolic bone disease, chronic widespread pain, and complex regional pain syndrome.
Featuring highly illustrated chapters, boxed summaries and links to further resources, ABC of Rheumatology is an accessible reference for all primary care health professional, general practitioners, family physicians, junior doctors, medical students and nurses.
Ade Adebajo FAcMed, FACP, FRCP(Glasg) is an Associate Director of Teaching at the University of Sheffield Medical School. He is also the Honorary Professor and Consultant Rheumatologist/Director of Undergraduate Medical Education, Faculty of Medicine for Dentistry and Health at University of Sheffield and Barnsley Hospital, South Yorkshire, UK.
Lisa Dunkley MBChB (Hons), FRCP, FHEA is a Consultant Rheumatologist TPD Rheumatology (S Yorks) at the Royal Hallamshire Hospital, Sheffield, UK.
ABC of Rheumatology continues to be a practical and informative guide to the assessment, treatment and management of common rheumatic and musculoskeletal conditions within primary care. Fully updated to reflect developments in this fast growing field, the fifth edition covers overviews of all key areas of rheumatology, and includes new chapters on radiology and immunology, as well as expanded coverage on metabolic bone disease, chronic widespread pain, and complex regional pain syndrome. Featuring highly illustrated chapters, boxed summaries and links to further resources, ABC of Rheumatology is an accessible reference for all primary care health professional, general practitioners, family physicians, junior doctors, medical students and nurses.
Ade Adebajo FAcMed, FACP, FRCP(Glasg) is an Associate Director of Teaching at the University of Sheffield Medical School. He is also the Honorary Professor and Consultant Rheumatologist/Director of Undergraduate Medical Education, Faculty of Medicine for Dentistry and Health at University of Sheffield and Barnsley Hospital, South Yorkshire, UK. Lisa Dunkley MBChB (Hons), FRCP, FHEA is a Consultant Rheumatologist TPD Rheumatology (S Yorks) at the Royal Hallamshire Hospital, Sheffield, UK.
Title Page 3
Copyright Page 6
Contents 7
Preface 9
Contributors 11
List of Abbreviations 15
Chapter 1 Delivering Musculoskeletal Care Across Boundaries 17
Introduction 17
Rheumatology in the community: the impact on primary care 17
Who should be referred to secondary care? 17
Musculoskeletal interface services 19
Further management 19
Conclusion 19
References 19
Chapter 2 Pain in the Wrist and Hand 21
Functional anatomy 21
Tendon problems 21
Flexor tenosynovitis 21
Finger flexor tendonosis and trigger finger 22
De Quervain’s tenosynovitis 22
Extensor tenosynovitis 23
Mallet finger 23
Dupuytren’s contracture 23
Peripheral nerve entrapment syndromes 24
Carpal tunnel syndrome 24
Cubital tunnel syndrome 24
Osteoarthritis 25
Nodal osteoarthritis 25
First carpometacarpal osteoarthritis 25
Systemic disorders causing hand pain 25
Inflammatory arthritis 25
Acute pseudogout and chondrocalcinosis of the wrist 25
Acute gout and chronic tophaceous gout 26
Diabetic stiff hand (cheiroarthropathy – limited joint mobility syndrome) 26
Raynaud’s phenomenon 26
Other disorders 26
Ganglion 26
Chronic (work-related) upper limb pain 26
Osteonecrosis (rare) 27
Scaphoid bone fracture 27
Writer’s cramp 27
Septic arthritis 27
Complex regional pain syndrome 27
Local corticosteroid injection technique 27
References 27
Further reading 27
Chapter 3 Pain in the Neck, Shoulder and Arm???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 29
Anatomy and function of the neck and shoulder joint 29
Clinical evaluation 29
Neck pain 30
Investigation of neck pain 31
Treatment of neck pain 31
Shoulder pain 32
Rotator cuff disease 33
Adhesive capsulitis 34
Other shoulder disorders 35
Elbow and forearm pain 36
Lateral and medial epicondylitis 36
Other elbow disorders 37
Reference 37
Further reading 37
Chapter 4 Low Back Pain?????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 39
Causes of low back pain 39
Lumbar spondylosis 39
Disc herniation 40
Spondylolisthesis 41
Spinal stenosis 41
Idiopathic (non-specific) low back pain 42
Neoplasms 42
Infection 42
Assessment 42
History 42
Physical examination 42
Imaging studies 43
Treatment 44
Acute low back pain 44
Chronic low back pain 45
Nerve root compression syndromes 45
Further reading 45
Chapter 5 Pain in the Hip?????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 47
Hip pain in children 47
Developmental dysplasia of the hip (DDH) 47
Perthes’ disease 47
Slipped upper femoral epiphysis (SUFE) 47
Septic arthritis 47
Transient synovitis/‘irritable hip’ 47
Other arthritides 48
Hip pain in adults 48
Osteoarthritis 48
Other arthritides 49
Hip fracture 49
Paget’s disease 49
Avascular necrosis 49
Malignancy 49
Femoro-acetabular impingement (FAI) 49
Painful soft tissue conditions around the hip 50
Management of hip pain 50
Acknowledgement 51
Further reading 51
Chapter 6 Pain in the Knee???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 53
Traumatic causes of knee pain 53
Meniscus injury 53
Articular cartilage injury 55
Differentiation of cause 55
Knee pain in younger people and athletes 55
Patellar tendonopathy 55
Anterior knee pain syndrome 55
Pes anserine bursitis 56
Iliotibial band friction syndrome 56
Knee pain in older people 56
Knee pain in systemic disease 57
Other causes of knee pain 58
‘Red flags’ 58
Further reading 58
Chapter 7 Pain in the Foot???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 59
Foot pain in children 59
Juvenile idiopathic arthritis 59
Pain in the forefoot (metatarsalgia) 60
Morton’s neuroma (interdigital neuroma) 60
Stress fracture (march fracture) 60
Acute synovitis 61
Differential diagnosis: inflammation of anterior metatarsal soft tissue pad 62
Plantar metatarsal bursitis 62
Pain along the medial longitudinal arch 62
Painful heel (Box 7.4) 62
Sever’s disease (calcaneal apophysitis) 62
Plantar calcaneal bursitis 63
Chronic inflammation of the heel pad 63
Achilles tendon affections 63
Osteochondritis 63
Arthropathies that affect the foot 64
Osteoarthritis 64
Rheumatoid arthritis 64
Spondyloarthritis 64
Neuropathic joint disease 64
Complex regional pain syndrome, type 1 64
Gout 66
Management of rheumatic foot conditions 66
Tissue viability 66
Foot function and joint protection 66
Foot health promotion 66
Foot surgery 66
Further reading 66
Chapter 8 Fibromyalgia Syndrome and Chronic Widespread Pain?????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 67
Diagnosis 67
Aetiology and symptoms 68
Investigations 68
Management 68
Education 68
Graded exercise 69
Pacing activities 69
Psychotherapeutic interventions 69
Sleep 69
Complementary/alternative medicine 69
Drug therapy 69
Conclusion 70
Further reading 70
Chapter 9 Osteoarthritis 71
Presentation 71
Symptoms 71
Examination 73
Investigations 73
Management 73
Patient education and information access 73
Exercise 74
Reducing adverse biomechanical factors 74
Pharmacological treatments 74
Surgery 74
Conclusion 76
References 76
Chapter 10 Gout, Hyperuricaemia and Crystal Arthritis 77
Gout and hyperuricaemia 77
Epidemiology 77
Risk factors for gout/hyperuricaemia 77
Relationship between gout and hyperuricaemia 79
Hyperuricaemia and cardiovascular disease 79
Clinical features 80
Acute gout 80
Chronic gout 80
Urate stones 80
Inherited metabolic disorders 80
Treatment 80
Acute gout 80
Intercritical and chronic gout 81
Pseudogout 81
Other crystal diseases 82
References 82
Further reading 82
Chapter 11 Osteoporosis and Metabolic Bone Disease???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 83
Normal physiology of bone 83
Osteoporosis 83
Assessment of osteoporosis 83
Reducing fracture risk 84
Pharmacological agents 85
Antiresorptive treatments 86
Anabolic treatments 86
In development 86
Pain relief and falls prevention 86
Monitoring of treatment 86
Osteomalacia 87
Paget’s disease of bone 87
Reference 88
Further reading 88
Chapter 12 Rheumatoid Arthritis: Clinical Features and Diagnosis???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 89
Pathogenesis 89
Clinical features 89
‘Red flags’ 90
Diagnosis 91
History 91
Clinical examination 91
Laboratory tests 91
Imaging 91
Synovial fluid analysis 92
Differential diagnosis 92
Further reading 92
Chapter 13 Treatment of Rheumatoid Arthritis???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 93
Non-steroidal anti-inflammatory drugs 93
Corticosteroids 93
Conventional disease-modifying antirheumatic drugs (DMARDs) 93
Gold 93
Methotrexate 94
Sulfasalazine 94
Hydroxychloroquine 94
Leflunomide 94
Combination therapy 94
Biological response modifiers 94
Tumour antagonists 94
Interleukin-1 receptor antagonist 95
B-cell depletion 95
Abatacept 95
Tocilizumab 95
Biosimilars 95
New small molecule DMARDs 95
Identification of co-existing problems 96
Complementary therapy 96
Further reading 96
Chapter 14 Spondyloarthritides???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 97
Axial spondyloarthritis/ankylosing spondylitis 97
Assessment of ankylosing spondylitis 99
Psoriatic arthritis 99
Reactive arthritis 101
Enteropathic arthritis 102
Undifferentiated spondyloarthritis 102
Treatment 102
Sacroiliitis and spondylitis 102
Oligoarthritis and/or enthesitis 103
Reference 103
Further reading 103
Chapter 15 Juvenile Idiopathic Arthritis???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 105
Epidemiology 105
Classification 105
Etiology 105
Pathogenesis 106
Oligoarthritis 106
Persistent oligoarthritis 106
Clinical features 106
Diagnosis 107
Extended oligoarthritis 107
Genetics 107
Prognosis 107
Uveitis 108
Epidemiology 108
Insidious-onset (chronic) uveitis 108
Suddenonset (acute) uveitis 108
Management of JIA-associated uveitis 108
Systemic juvenile idiopathic arthritis 108
Pathogenesis 109
Extra-articular clinical features 109
Central nervous system disease 109
Musculoskeletal manifestations 110
Diagnosis and differential diagnosis 110
Features seen during the course of the disease 110
Systemic complications 110
Prognosis 111
Polyarticular juvenile idiopathic arthritis 111
Rheumatoid factor-negative polyarthritis 111
Rheumatoid factor-positive polyarthritis 112
Psoriatic arthritis 112
Pathogenesis 112
Clinical features 112
Laboratory examination 113
Prognosis 113
Enthesitis-related arthritis 113
Epidemiology and pathogenesis 114
Clinical features 114
Systemic features 114
Investigations (Box 15.9) 114
Prognosis 114
Undifferentiated arthritis 114
Treatment of juvenile idiopathic arthritis 115
Non-steroidal anti-inflammatory drugs 115
Corticosteroids 115
DMARDs 115
Biologic drugs 115
References 117
Further reading 117
Chapter 16 Musculoskeletal Disorders in Children and Adolescents???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 119
The ‘limping child’ 119
Back pain 119
Mechanical pain 121
Neoplasia 122
Arthritis and infection 122
Chronic arthritis (JIA) 123
Connective tissue diseases 123
Systemic lupus erythematosus 123
Juvenile dermatomyositis 123
Sclerodermas 124
Vasculitis 125
Rare inflammatory syndromes 126
Inherited autoinflammatory syndromes 126
The role of the multidisciplinary team 126
References 127
Further reading 127
Chapter 17 Polymyalgia Rheumatica and Giant Cell Arteritis 129
Epidemiology 129
Clinical features and diagnosis 129
Making the diagnosis 131
Treatment of PMR and GCA 132
Monitoring PMR and GCA 133
References 133
Chapter 18 Systemic Lupus Erythematosus and Lupus-Like Syndromes???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 135
Causes 135
Epidemiology 136
Clinical presentations 136
Systemic lupus erythematosus 136
General features 137
Mucocutaneous manifestations 137
Musculoskeletal manifestations 137
Haematological manifestations 137
Renal manifestations 138
Nervous system manifestations 138
Pulmonary and cardiovascular manifestations 139
Gastrointestinal manifestations 139
Pregnancy and systemic lupus erythematosus 139
Neonatal lupus syndrome 139
Sjögren’s syndrome 139
Overlap syndromes and other lupus?like conditions 140
Polymyositis and dermatomyositis 140
Antiphospholipid syndrome 140
Thrombosis 140
Obstetric syndromes 140
Other manifestations 140
Catastrophic antiphospholipid syndrome 141
Outcome of systemic lupus erythematosus and antiphospholipid syndrome 141
Investigations 141
Investigations in systemic lupus erythematosus 141
Investigations in antiphospholipid syndrome 141
Management 141
General measures 141
Drug therapy in systemic lupus erythematosus (Bertsias et al., 2012 Mosca et al., 2010)
Biologic treatments currently used in lupus 143
Therapy in antiphospholipid antibody syndrome (Box 18.8) 143
Conclusion 143
References 143
Chapter 19 Raynaud’s Phenomenon and Scleroderma?????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 145
Diagnosis, classification and epidemiology of scleroderma 145
Raynaud’s phenomenon and connective tissue disease 145
Systemic sclerosis 146
Diffuse cutaneous systemic sclerosis (dcSSc) 146
Limited cutaneous systemic sclerosis (lcSSc) 148
Aetiopathogenesis 148
Autoantibody profiles 148
Risk stratification in systemic sclerosis 149
Management of systemic sclerosis 149
Organ-based complications 150
Conclusion 152
Further reading 152
Resource 152
Chapter 20 Reflex Sympathetic Dystrophy 153
Introduction 153
What causes RSD? 153
How is RSD diagnosed? 154
How is RSD treated? 155
Reference 156
Further reading 156
Chapter 21 Is It an Autoimmune Rheumatic Disease??????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 157
Autoantibody profile in diagnosis 157
Which systemic autoimmune rheumatic disease? 158
Differential diagnosis 160
Drug-induced lupus 160
Other disorders of the skin 161
Fibromyalgia 162
Endocrine disorders 162
Is it infection? 163
Reference 163
Further reading 163
Chapter 22 Sport and Exercise Medicine???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 165
Sports injuries 165
‘Know the patient, know the sport, know the injury’ 165
Assessment 165
Management (Box 22.1) 166
Common sports injuries – the acute injury 167
Common sports injuries – the chronic/overuse injury 168
Exercise prescription 169
Summary 169
Further reading 169
Chapter 23 Vasculitis and Related Rashes???????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 171
Large-vessel vasculitis 172
Medium-vessel vasculitis 172
Polyarteritis nodosa 172
Kawasaki’s disease (mucocutaneous lymph node syndrome) 172
Medium- and small-vessel vasculitis 172
Granulomatosis with polyangiitis (Wegener’s) 172
Microscopic polyangiitis 173
Eosinophilic granulomatosis with polyangiitis (Churg–Strauss) 173
Small-vessel vasculitis 173
IgA vasculitis (Henoch–Schönlein purpura) 173
Behçet’s disease 173
Investigation 173
Urine analysis 174
Blood tests 174
Liver function tests 174
Immunology 174
Biopsy 174
Other investigations 174
Differential diagnosis 174
Livedo reticularis 174
Bacterial infections 174
Infective endocarditis 174
Cholesterol embolism 175
Atrial myxoma 175
Antiphospholipid antibody syndrome 175
Cocaine abuse 175
Prognosis 175
Treatment 175
Further reading 176
Chapter 24 Basic Immunology and the Biologic Era 177
Inflammation 177
Activation of the adaptive immune response 177
Cells of the immune system 177
T-cells 177
B-cells 178
Macrophages 179
Biologic therapies 179
Structure 181
Cytokine-based treatments 181
Cell depletion 182
Co-stimulation blockade 182
Efficacy 182
Safety 182
Anti-drug antibodies 184
Biosimilars 184
Janus kinase inhibition 184
Further reading 184
Chapter 25 Laboratory Tests 185
Haematology investigations 185
Anaemia 185
Platelet abnormalities 185
White blood cell abnormalities 186
Acute-phase response 186
Biochemical investigations 187
Hepatic function 187
Renal function 188
Bone biochemistry 188
Other biochemical tests 188
Immunological tests 188
Autoantibodies 188
Rheumatoid factors 189
Antibodies to cyclic citrullinated peptides 189
Antinuclear antibodies 189
Antibodies to DNA 189
Antibodies to extractable nuclear antigens 190
Antiphospholipid antibodies 191
Antineutrophil cytoplasmic antibodies 191
Immunoglobulins 191
Complement 192
Genetic associations 192
Microbiology 192
Further reading 192
Chapter 26 Musculoskeletal Radiology 193
Plain radiography (X-ray) 193
Ultrasound scanning 197
Magnetic resonance imaging 198
Computed tomography 198
Bone scintigraphy 199
Positron emission tomography 199
Dual energy X-ray absorptiometry 200
Further reading 200
Chapter 27 The Team Approach 201
The patient as a member of the multidisciplinary team 201
Effectiveness of multidisciplinary team working 202
Roles and responsibilities of members of the team 202
Consultant and medical staff 202
Rheumatology nurse specialist 202
Occupational therapist 202
Physiotherapist 203
Podiatrist 203
Other members of the MDT 203
Charity organizations 203
Further reading 204
Chapter 28 Epidemiology of the Rheumatic Diseases 205
Osteoarthritis 205
Musculoskeletal pain 205
Low back pain 205
Neck pain 207
Chronic widespread pain and fibromyalgia 207
Gout 207
Rheumatoid arthritis 207
Spondyloarthritis 208
Ankylosing spondylitis 208
Psoriatic arthritis 208
Connective tissue disease 209
Systemic lupus erythematosus 209
Scleroderma 209
Polymyalgia rheumatica and giant cell arteritis 209
Osteoporosis 209
Index 211
EULA 226
| Erscheint lt. Verlag | 14.3.2018 |
|---|---|
| Reihe/Serie | ABC Series | ABC Series |
| Sprache | englisch |
| Themenwelt | Medizinische Fachgebiete ► Innere Medizin ► Rheumatologie |
| Schlagworte | Allgemeine u. Innere Medizin • Allgemeinpraxis, hausärztliche Praxis • assessment of common musculoskeletal conditions • assessment of common rheumatic conditions • General & Internal Medicine • General Practice/Family Practice • <p>guide to rheumatology • management of common rheumatic and musculoskeletal conditions • Medical Science • Medizin • overviews of key areas of rheumatology</p> • practical guide to rheumatology • Rheumatologie • rheumatology • treatment of common musculoskeletal conditions • treatment of common rheumatic conditions • treatment of common rheumatic conditions within primary care |
| ISBN-10 | 1-118-79318-8 / 1118793188 |
| ISBN-13 | 978-1-118-79318-3 / 9781118793183 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: PDF (Portable Document Format)
Mit einem festen Seitenlayout eignet sich die PDF besonders für Fachbücher mit Spalten, Tabellen und Abbildungen. Eine PDF kann auf fast allen Geräten angezeigt werden, ist aber für kleine Displays (Smartphone, eReader) nur eingeschränkt geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich