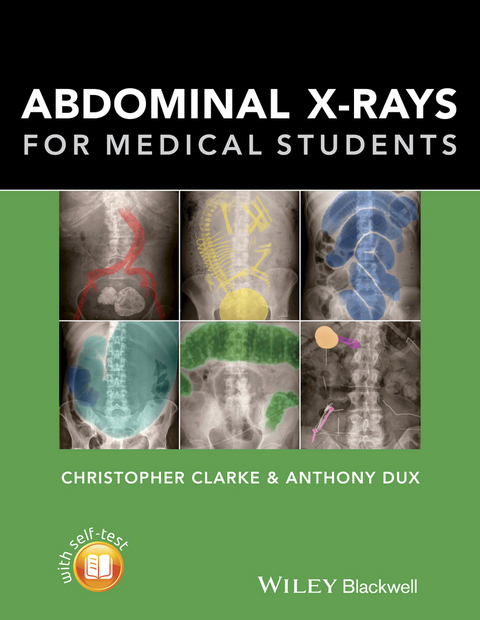
Abdominal X-rays for Medical Students (eBook)
John Wiley & Sons (Verlag)
978-1-118-60054-2 (ISBN)
Highly Commended at the British Medical Association Book Awards 2016
Abdominal X-rays for Medical Students is a comprehensive resource offering guidance on reading, presenting and interpreting abdominal radiographs. Suitable for medical students, junior doctors, nurses and trainee radiographers, this brand new title is clearly illustrated using a unique colour overlay system to present the main pathologies and to highlight the abnormalities in abdomen x-rays.
Abdominal X-rays for Medical Students:
- Covers the key knowledge and skills necessary for practical use
- Provides an effective and memorable way to analyse and present abdominal radiographs - the unique 'ABCDE' system as developed by the authors
- Presents each radiograph twice, side by side: the first as seen in the clinical setting, and the second with the pathology clearly highlighted
- Includes self-assessment to test knowledge and presentation technique
With a systematic approach covering both the analysis of radiographs and next steps mirroring the clinical setting and context, Abdominal X-rays for Medical Students is a succinct and up-to-date overview of the principles and practice of this important topic.
Christopher Clarke is Radiology Registrar and Honorary Lecturer in Human Anatomy, Nottingham University Hospitals
Anthony Dux is a former Consultant Radiologist and Honorary Senior Lecturer, University Hospitals of Leicester
Christopher Clarke is Radiology Registrar and Honorary Lecturer in Human Anatomy, Nottingham University Hospitals Anthony Dux is a former Consultant Radiologist and Honorary Senior Lecturer, University Hospitals of Leicester
Preface vii
Acknowledgements viii
Learning objectives checklistix
Part 1 About X-rays 1
What are X-rays? 1
How are X-rays produced? 1
How do X-rays make an image? 2
How are X-ray images (radiographs) stored? 3
Radiation hazards 3
The Ionising Radiation (Medical Exposure) Regulations 3
In women of reproductive age 3
Indications for an abdominal X-ray 4
Abdominal X-ray views 5
AP Supine abdominal X-ray 5
Other views 5
Radiograph quality 6
Inclusion 6
Exposure 6
Normal anatomy on an abdominal X-ray 8
Right and left (Figure 7) 8
Quadrants and regions (Figure 8) 8
Abdominal viscera 1 (Figure 9) 8
Abdominal viscera 2 (Figure 10) 9
Skeletal structures (Figure 11) 10
Pelvis (Figure 12) 10
Lung bases (may be visualised at the top of the abdomen) (Figure 13) 11
Bowel 1 (Figure 14) 11
Bowel 2 (Figure 15) 12
Presenting an abdominal radiograph 14
Be systematic! 14
Part 2 Overview of the ABCDE of abdominal radiographs 15
A - Air in the wrong place 16
Pneumoperitoneum (gas in the peritoneal cavity) 21
Pneumoretroperitoneum (gas in the retroperitoneal space) 26
Pneumobilia (gas in the biliary tree) 28
Portal venous gas (gas in the portal vein) 29
B - Bowel 17
Dilated small bowel 30
Dilated large bowel 34
Volvulus 37
Dilated stomach 40
Hernia 41
Bowel wall inflammation 43
Faecal loading 48
Faecal impaction 49
C - Calcification 18
Gallstones in the gallbladder (cholelithiasis) 50
Renal stones (urolithiasis) 53
Bladder stones 56
Nephrocalcinosis 57
Pancreatic calcification 58
Adrenal calcification 59
Abdominal aortic aneurysm (AAA) calcification 60
Fetus 62
Calcified structures of little clinical significance 63
Calcified costal cartilage 63
Phleboliths ('vein stones') 63
Calcified mesenteric lymph nodes 64
Calcified uterine fibroids 65
Prostate calcification 65
Abdominal aortic calcification (normal calibre) 66
Splenic artery calcification 66
D - Disability (bones and solid organs) 19
Pelvic fractures - 3 Polo rings test 67
Sclerotic and lucent bone lesions 68
Spine pathology 69
Solid organ enlargement 71
E - Everything else 20
Medical and surgical objects (iatrogenic) 73
Surgical clips/staples/sutures 73
Urinary catheter 75
Supra-pubic catheter 75
Nasogastric (NG) and nasojejunal (NJ) tubes 76
Flatus tube 77
Surgical drain 78
Nephrostomy catheter 78
Peritoneal dialysis (PD) catheter 79
Gastric band device 79
Percutaneous endoscopic gastrostomy (PEG)/ radiologically inserted gastrostomy (RIG) 80
Stoma bag 80
Stents 81
Inferior vena cava (IVC) filter 84
Intra-uterine device (IUD) 85
Pessary 85
Foreign bodies 86
Retained surgical swab 86
Swallowed objects 87
Objects inserted per-rectum (PR) 88
Clothing artefact 90
Piercings 90
Body packer 91
Lung bases 93
Self-assessment questions 94
Self-assessment answers 99
Glossary 107
Index 112
Overview of the ABCDE of abdominal radiographs
It is important to use a systematic approach when looking at an abdominal radiograph. The following ABCDE approach is easy to remember, so when it comes to your exams and you have a moment of panic after being asked to talk about an abdominal X-ray, you can stick to these basics, even if you don’t have a clue what’s going on!
A is for Air in the wrong place
- Look for pneumoperitoneum and pneumoretroperitoneum
- Look for gas in the biliary tree and portal vein
B is for Bowel
- Look for dilated small and large bowel
- Look for a volvulus
- Look for a distended stomach
- Look for a hernia
- Look for evidence of bowel wall thickening
C is for Calcification
- Look for clinically significant calcified structures such as calcified gallstones, renal calculus, nephrocalcinosis, pancreatic calcification and an abdominal aortic aneurysm (AAA)
- Look for a foetus (females)
- Look for clinically insignificant calcified structures such as costal cartilage calcification, phleboliths, mesenteric lymph nodes, calcified fibroids, prostate calcification and vascular calcification
D is for Disability (bones and solid organs)
- Look at the bony skeleton for fractures and sclerotic/lytic bone lesions
- Look at the spine for vertebral body height, alignment, pedicles and a ‘bamboo spine’
- Look for solid organ enlargement
E is for Everything else
- Look for evidence of previous surgery and other medical devices
- Look for foreign bodies
- Look at the lung bases
A – Air in the wrong place
How to look?
- Look for free gas in the peritoneal cavity (pneumoperitoneum). To do this, look for Rigler’s sign (gas present on both sides of the intestinal wall), gas outlining the liver and look to see if the falciform ligament is visible.
- Look for free gas in the retroperitoneum (pneumoretroperitoneum). To do this, look specifically for gas outlining the kidneys.
- Look at the liver (right upper quadrant) for linear areas of increased lucency. Gas seen towards the centre of the liver indicates gas in the biliary tree (pneumobilia), for example within the common bile duct (CBD), hepatic ducts and/or gallbladder. Gas seen towards the periphery of the liver indicates gas in the portal vein.
What to look for in A – Air in the wrong place?
| Pneumoperitoneum (gas in the peritoneal cavity) | p. 21 |
| Pneumoretroperitoneum (gas in the retroperitoneal space) | p. 26 |
| Pneumobilia (gas in the biliary tree) | p. 28 |
| Portal venous gas (gas in the portal vein) | p. 29 |
B – Bowel
How to look?
- Look at the bowel loops for small or large bowel dilatation.
- Look for a very large dilated loop of bowel that could represent a sigmoid or caecal volvulus. If the dilated bowel loop is in the upper abdomen, consider whether it may represent a distended stomach.
- Look at the left and right iliac regions for any bowel gas seen projected below the level of the inguinal ligament suggesting an inguinal or femoral hernia.
- Look for thickening of the bowel wall to suggest bowel wall inflammation. Specifically look for thumbprinting and the characteristic lead pipe colon.
What to look for in B – Bowel?
| Dilated small bowel | p. 30 |
| Dilated large bowel | p. 34 |
| Volvulus | p. 37 |
| Dilated stomach | p. 40 |
| Hernia | p. 41 |
| Bowel wall inflammation | p. 43 |
| Faecal loading | p. 48 |
| Faecal impaction | p. 49 |
C – Calcification
How to look?
- Look at the right upper quadrant for calcified gallstones (blue).
- Look over the course of the kidneys and ureters for renal stones (green) and look specifically in the region of both kidneys for a staghorn calculus or nephrocalcinosis (light green).
- Look at the suprapubic region for bladder stones (yellow).
- Look at the upper central abdomen for pancreatic calcification (light blue).
- Look in the regions of the upper poles of both kidneys for adrenal calcification (pink).
- Look at the umbilical region for abdominal aortic aneurysm (AAA) calcification (red).
- In a female patient, look for a foetus (‘skeleton with the abdomen’ appearance).
Figure 16: Diagrammatic representation of key areas to review when looking for abnormal calcification.
What to look for in C – Calcification?
| Gallstones in the gallbladder (cholelithiasis) | p. 50 |
| Renal stones (urolithiasis) | p. 53 |
| Bladder stones | p. 56 |
| Nephrocalcinosis | p. 57 |
| Pancreatic calcification | p. 58 |
| Adrenal calcification | p. 59 |
| Abdominal aortic aneurysm (AAA) calcification | p. 60 |
| Fetus | p. 62 |
Also look for clinically insignificant calcified structures such:
| Calcified costal cartilage | p. 63 |
| Phleboliths (‘vein stones’) | p. 63 |
| Calcified mesenteric lymph nodes | p. 64 |
| Calcified uterine fibroids | p. 65 |
| Prostate calcification | p. 65 |
| Abdominal aortic calcification (normal calibre) | p. 66 |
| Splenic artery calcification | p. 66 |
D – Disability (bones and solid organs)
How to look?
- Look at the bony pelvis for a fracture (#). If a fracture is seen, use the 3 Polo rings test to look for a second fracture (or disruption of the pubic symphysis or sacroiliac joints).
- Look for a sclerotic (increased density) or lucent (reduced density) bone lesion.
- Look at the spine for loss of vertebral body height, loss of visualisation of a pedicle, loss of normal alignment (e.g. scoliosis) and bamboo spine (ankylosing spondylitis).
- Look over the whole radiograph for any evidence of solid organ enlargement.
What to look for in D – disability (bones and soft tissues)?
| Pelvic fractures – 3 Polo rings test | p. 67 |
| Sclerotic and lucent bone lesions | p. 68 |
| Spine pathology | p. 69 |
| Solid organ enlargement | p. 71 |
E – Everything else
How to look?
- Look at the whole radiograph for any evidence of previous surgery such as surgical staples, clips, hernia clips or bowel anastomoses.
- Look for any catheters, drains, stents or other tubing (e.g. gastric band or gastrostomy feeding tube).
- Look in the pelvis for an intra-uterine device (IUD) or pessary.
- Look carefully for any foreign bodies.
- Look at the lung bases for lung metastasis or other lung pathology.
What to look for in E – everything else?
| Medical and surgical objects (iatrogenic) | p. 73 |
| Surgical clips/staples/sutures | p. 73 |
| Urinary catheter | p. 75 |
| Supra-pubic catheter | p. 75 |
| Nasogastric (NG) and nasojejunal (NJ) tubes | p. 76 |
| Flatus tube | p. 77 |
| Surgical drain | p. 78 |
| Nephrostomy catheter | p. 78 |
| Peritoneal dialysis (PD) catheter | p. 79 |
| Gastric band device | p. 79 |
| Percutaneous endoscopic gastrostomy (PEG)/radiologically inserted gastrostomy (RIG) | p. 80 |
| Stoma bag | p. 80 |
| Stents | p. 81 |
| Inferior vena cava (IVC) filter | p. 84 |
| Intra-uterine device... |
| Erscheint lt. Verlag | 27.2.2015 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Gesundheitsfachberufe |
| Medizinische Fachgebiete ► Radiologie / Bildgebende Verfahren ► Radiologie | |
| Schlagworte | Abdomen • abdominal xrays x-ray imaging medical student reading presenting radiography radiographs junior doctors nurses trainee radiographer pathologies abnormalities • Medical Science • Medizin • Medizinstudium • Radiologie • Radiologie u. Bildgebende Verfahren • Radiology & Imaging • Röntgenaufnahme • Röntgenaufnahme |
| ISBN-10 | 1-118-60054-1 / 1118600541 |
| ISBN-13 | 978-1-118-60054-2 / 9781118600542 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich