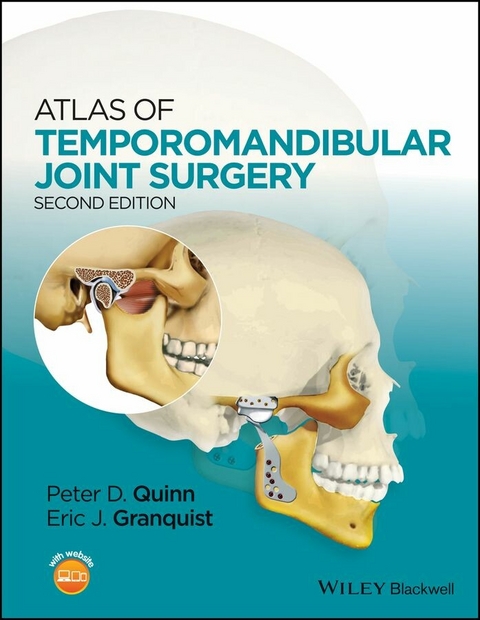
Atlas of Temporomandibular Joint Surgery (eBook)
John Wiley & Sons (Verlag)
978-1-118-82525-9 (ISBN)
This second edition of the Atlas of Temporomandibular Joint Surgery is a major revision of Dr. Quinn's classic work, taking into account new procedures, equipment, and evidence-based findings from the latest research in TMJ treatment.
Assuming that readers are familiar with non-surgical therapies to correct temporomandibular pain and disorders, Drs. Quinn and Granquist focus on the surgical remedies for disorders that are beyond conservative treatment. This concise, how-to surgical atlas guides both the novice and experienced surgeon through the intra-articular and extra-articular procedures that have proven efficacious in the treatment of advanced craniomandibular dysfunction. Chapters take readers through decision making for TMJ surgery, diagnostic imaging methods, surgical approaches, surgery for internal derangements, trauma, osseous surgical procedures, total joint replacement, and pathologies.
Peter D. Quinn, DMD, MD, is the Schoenleber Professor of Oral and Maxillofacial Surgery at the University of Pennsylvania School of Dental Medicine. In addition, he is currently Vice Dean of Professional Services at the University of Pennsylvania Perelman School of Medicine and Senior Vice President for the University of Pennsylvania Health System. He previously served as Chair of the Department of Oral and Maxillofacial Surgery at the dental school and at the Hospital of the University of Pennsylvania from 1986 to 2008. Dr. Quinn was the principal and lead developer of the Biomet Total Mandibular Joint Replacement System, the most widely used alloplastic prosthesis in the world.
Eric J. Granquist, DMD, MD, completed his surgical training at the Hospital of the University of Pennsylvania and is currently an Assistant Professor at the University of Pennsylvania School of Dental Medicine. Dr. Granquist's primary interest is in temporomandibular surgery and translational research. His current work includes the investigation of biomarkers in osteoarthritis of the TMJ as well as the development of novel imaging modalities of the temporomandibular joint. In addition to this work, he is also the principal investigator in several clinical trials involving the surgical treatment of the TMJ. Dr. Granquist has an active clinical practice at the Hospital of the University of Pennsylvania, Children's Hospital of Philadelphia, and Philadelphia Veteran's hospital.
This second edition of the Atlas of Temporomandibular Joint Surgery is a major revision of Dr. Quinn s classic work, taking into account new procedures, equipment, and evidence-based findings from the latest research in TMJ treatment. Assuming that readers are familiar with non-surgical therapies to correct temporomandibular pain and disorders, Drs. Quinn and Granquist focus on the surgical remedies for disorders that are beyond conservative treatment. This concise, how-to surgical atlas guides both the novice and experienced surgeon through the intra-articular and extra-articular procedures that have proven efficacious in the treatment of advanced craniomandibular dysfunction. Chapters take readers through decision making for TMJ surgery, diagnostic imaging methods, surgical approaches, surgery for internal derangements, trauma, osseous surgical procedures, total joint replacement, and pathologies.
Peter D. Quinn, DMD, MD, is the Schoenleber Professor of Oral and Maxillofacial Surgery at the University of Pennsylvania School of Dental Medicine. In addition, he is currently Vice Dean of Professional Services at the University of Pennsylvania Perelman School of Medicine and Senior Vice President for the University of Pennsylvania Health System. He previously served as Chair of the Department of Oral and Maxillofacial Surgery at the dental school and at the Hospital of the University of Pennsylvania from 1986 to 2008. Dr. Quinn was the principal and lead developer of the Biomet Total Mandibular Joint Replacement System, the most widely used alloplastic prosthesis in the world. Eric J. Granquist, DMD, MD, completed his surgical training at the Hospital of the University of Pennsylvania and is currently an Assistant Professor at the University of Pennsylvania School of Dental Medicine. Dr. Granquist's primary interest is in temporomandibular surgery and translational research. His current work includes the investigation of biomarkers in osteoarthritis of the TMJ as well as the development of novel imaging modalities of the temporomandibular joint. In addition to this work, he is also the principal investigator in several clinical trials involving the surgical treatment of the TMJ. Dr. Granquist has an active clinical practice at the Hospital of the University of Pennsylvania, Children's Hospital of Philadelphia, and Philadelphia Veteran's hospital.
Contributors list vii
Preface ix
Acknowledgments xi
About the companion website xiii
1 Surgical decision making for temporomandibular joint surgery 1
2 Diagnostic imaging of the temporomandibular joint 5
3 Surgical approaches to the temporomandibular joint 31
4 Surgery for internal derangements 57
5 Osseous surgery of the temporomandibular joint 85
6 Trauma 105
7 Autogenous reconstruction of the temporomandibular joint 131
8 Stock alloplastic reconstruction of the temporomandibular joint 145
9 Custom alloplastic reconstruction of the temporomandibular joint 181
10 Pathology of the temporomandibular joint 203
11 Complications 231
Index 245
CHAPTER 2
Diagnostic imaging of the temporomandibular joint
Because of the anatomic complexity of the temporomandibular joint (TMJ) and its proximity to the base of the skull, temporal bone, mastoid air cells, and auditory structures, imaging of the joint structures can be problematic. Imaging studies should aid the clinician in diagnosis and surgical planning. The choice of imaging modality should be based on history and physical exam. Consideration should be given to the amount of radiation, invasiveness of the exam, ability to obtain the study, and cost. The study that is able to best answer the clinical question while maximizing cost effectiveness should be utilized.
Plain film, tomograms, and orthopantogram radiography
Plain films, tomograms, and orthopantogram (panoramic) studies provide good osseous detail of the TMJ, with minimal radiation, and are easily obtained. As such, they are often an excellent choice for initial evaluation of TMJ pathology.
Standard transcranial (lateral oblique) views provide a global view of bony architecture of the articular surfaces. If possible, a submental vertex film can be taken to allow the lateral oblique transcranial projection to be angled directly through the long access of the condyle. This improves the image quality and also allows standardization of subsequent transcranial views. With the exception of emergency room visits for trauma or dislocation, tomograms or panoramic radiographs have largely replaced these studies.
Tomography has been widely available since the early 1940s and provides finer detail for the examination of osseous abnormalities than detected by plain film techniques. The angle-corrected tomograms for sagittal tomography are recommended so that the sectioning is always perpendicular to the long axis of the condyle. This gives a truer picture of the condyle position, gives the best evaluation of erosion and osteophyte formation, and allows subsequent comparative studies to be performed by use of a standard method. The angle can be determined by measuring the angle between the condylar axis and a horizontal baseline on a submental vertex view.
Orthopantogram radiographs have been described as “curved tomograms.” They are, in fact, laminograms of a single plane. This study provides osseous imaging of the condyle and fossa, includes both joints, as well as the entire mandible for comparison of symmetry. Disadvantages include “ghost” images, distortion (~20%), and less detail when compared to angle-corrected condylar tomograms. Newer units allow for separate positioning of right and left joints, creating more correct placement of the condyle in the zone of focus, improving resolution. Some units are able to produce tomograms, allowing increased anatomic detail of the condyle.
Figure 2.1 Transcranial radiograph, demonstrating the limitations of this study. Note the overlap of adjacent structures with the glenoid fossa and mandibular condyle.
Figure 2.2 (a) Later oblique in the closed mouth position, note mandibular condyle seated in the glenoid fossa (inset). (b) Lateral oblique in open mouth position, note translation of TMJ condyle (inset).
Plain films and tomographic images are beneficial in assessing osseous changes in the condyle and eminence. However, the use of these films to assess condylar position with any accuracy is questionable at best. Several studies have shown that the position of the condyle, as depicted in these radiographic techniques, is of little clinical significance. Open- and closed-mouth tomographic views can provide valuable information with regard to condylar translation. Although it has been postulated that during normal range of motion the greatest convexity of the condyle reaches the greatest convexity of the articular eminence, several studies have shown that a majority of patients actually can translate beyond the greatest convexity of the articular eminence without subluxation, dislocation, or any symptoms. These studies can diagnose restricted range of motion but do not provide enough information to determine the etiology of that restriction.
Figure 2.3 Lateral cephalogram showing bilateral dislocation of the temporomandibular joints. Note anteriorly positioned mandible and open bite.
Figure 2.4 Postoperative lateral cephalogram. Study demonstrates good condylar prosthetic position and occlusal relationship.
Figure 2.5 (a) Preoperative posterior–anterior (PA) skull film. Note facial asymmetry involving the maxilla and mandible. (b) Postoperative PA demonstrating achievement of facial symmetry. Condylar prosthesis is well aligned. Note maxillary hardware from Le Fort I procedure.
Figure 2.6 (a) Patient positioned for angle-corrected temporomandibular joint tomograms.
Source: Quinn 1998, figure 2.3a, p. 7. Reproduced with permission of Elsevier.
(b) Angle-corrected tomogram of right temporomandibular joint.
Figure 2.7 Tomographic technique—basic principle of tomographic X-rays. Both the radiation source and film are moving simultaneously to blur all the anatomy anterior and posterior to the point of plane convergence.
Figure 2.8 Representation of sagittal cuts in standard tomographic condylar films showing anatomy from the most lateral to the most medial cut (a) progressing medial (b, c, d) to the most medial cut (e).
Figure 2.9 Typical contours of lateral condylar tomograms in varying stages of degenerative joint disease.
Figure 2.10 (a) Temporomandibular joint-tomographic series depicting excellent osseous detail with 5 mm cuts. (b) Sclerosis and condylar head flatting. (c) “Bird-beaking” of condyle in late stage degeneration.
Figure 2.11 (a) Patient positioned for panoramic tomogram of the temporomandibular joints. (b) Example of programmed condylar views available on most panoramic tomographic units. (c) Bilateral positioning techniques for specific temporomandibular joint-panoramic X-ray imaging positioned to align the condyle into the center of the “trough” of resolution of the panoramic tomogram.
Arthrography
Magnetic resonance imaging (MRI) has replaced arthrography in most instances for soft tissue imaging of the TMJ. Arthrography can offer valuable information not always available through any other imaging technique. It is the only imaging technique that demonstrates perforations in the disk in “real-time” because the operator can see the dye escape from the inferior to the superior joint space during the initial injection. The usual technique involves injection of a water-soluble, iodinated contrast material into the inferior joint space under fluoroscopy. A videotaped arthrofluoroscopic study could clearly show the various stages of disk displacement with or without reduction but is unable to show medial or lateral disk displacement. Potential complications from arthrography include allergic reaction to the contrast material, infection, and pain and swelling secondary to the invasive puncture technique used during the procedure.
Figure 2.12 (a) Dedicated tomogram showing bilateral degenerative joint disease, note the subchondral cyst on the right condyle (arrow). (b) Panorex of same patient. Note improved anatomic detail is evident in the tomogram (a) when compared to the panorex (b).
Figure 2.13 Panorex demonstrating left TMJ “bird beaking” and condylar sclerosis.
Figure 2.14 Patient with temporomandibular joint osteoarthritis prior to the completion of facial growth. Note decreased ramus height (double arrow) and increased premasseteric (antegonial) notching (single arrow).
Figure 2.15 “Hoof” deformity in condylar head, secondary to condylar trauma during growth. Panorex (a) and status-post resection (b).
Figure 2.16 (a) Panorex of a pediatric patient with ankylosis of the temporomandibular joint. Note displaced condylar head superior to the sigmoid notch (arrow). (b) Intraoperative photo of the same patient showing the ankylosis and fibrous union of the condyle to the skull base.
Figure 2.17 (a) Preoperative panorex of a patient with facial asymmetry secondary to temporomandibular juvenile rheumatoid arthritis. (b) Immediate postoperative panorex following total joint replacement, Le Fort I osteotomy and genioplasty.
Figure 2.18 (a) Coronal computer-tomography (CT) in bone windows, showing normal temporomandibular joints. (b) Sagittal CT in bone windows, showing a normal temporomandibular joint.
Figure 2.19 Coronal CT showing early erosion of the left condyle in a patient with osteoarthritis.
Computer tomography, 3D reconstruction, and computer planning
Computer tomography (CT) of the TMJ is currently the best method for assessing bony pathologic conditions of the TMJ and allows assessment of the proximity of surrounding vital structures for surgical planning. Most modern scanners are able to produce fine cuts of the area of interest, which allows for reconstruction of...
| Erscheint lt. Verlag | 24.2.2015 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Gesundheitsfachberufe |
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Chirurgie | |
| Medizin / Pharmazie ► Zahnmedizin ► Chirurgie | |
| Schlagworte | dentistry • joint replacement • maxillofacial surgery • Mund-, Kiefer- u. Gesichtschirurgie • Oral & Maxillofacial Surgery • Oral Surgery,?Oral & Maxillofacial Surgery • Orofacial Pain • Plastic and Reconstructive Surgery • Surgery • Temporomandibular disorders • temporomandibular joint • Temporomandibular Joint Surgery • TMD • TMJ • TMJ DIsorders • TMJ Joint replacement • TMJ reconstruction • TMJ Surgery • Trauma • Zahnmedizin |
| ISBN-10 | 1-118-82525-X / 111882525X |
| ISBN-13 | 978-1-118-82525-9 / 9781118825259 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich