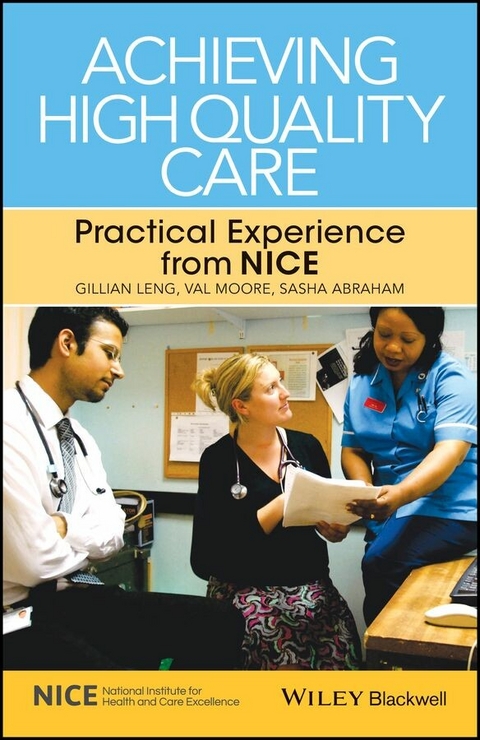
Achieving High Quality Care (eBook)
John Wiley & Sons (Verlag)
978-1-118-54358-0 (ISBN)
Drawing on the experience of the National Institute for Health and Care Excellence (NICE), Achieving High Quality Care is a practical guide on how to recognise and implement high quality evidence and guidance.
This new title provides an overview of the evidence behind successful initiatives designed to change practice and improve the quality of health care. It provides an overall picture of change management, from understanding the barriers to change to how these barriers can best be overcome. It presents a concise summary of the evidence for change, plus examples of specific initiatives drawn from experience of putting NICE guidance into practice.
The book includes a wide range of examples of positive change - plus key practical points highlighted throughout the text - to help readers achieve improvements in patient care. Finally, it shows how to measure change, assess improvement to agreed standards and to manage the ongoing process of change towards improving health care.
Achieving High Quality Care is a helpful guide for busy health care professionals wanting to improve services and patient care. It is relevant to everyone involved in the organisation and provision of quality health care, including clinicians and health care managers, who are trying to lead change and improve care through implementing evidence-based guidance.
Gillian Leng, Deputy Chief Executive, National Institute for Health and Care Excellence, London, UK; Visiting Professor, King’s College London, Division of Health and Social Research, London, UK
Val Moore, Implementation Programme Director, National Institute for Health and Care Excellence, London, UK
Sasha Abraham, General Practitioner, Tower Hamlets, London, UK
Drawing on the experience of the National Institute for Health and Care Excellence (NICE), Achieving High Quality Care is a practical guide on how to recognise and implement high quality evidence and guidance.This new title provides an overview of the evidence behind successful initiatives designed to change practice and improve the quality of health care. It provides an overall picture of change management, from understanding the barriers to change to how these barriers can best be overcome. It presents a concise summary of the evidence for change, plus examples of specific initiatives drawn from experience of putting NICE guidance into practice.The book includes a wide range of examples of positive change - plus key practical points highlighted throughout the text - to help readers achieve improvements in patient care. Finally, it shows how to measure change, assess improvement to agreed standards and to manage the ongoing process of change towards improving health care.Achieving High Quality Care is a helpful guide for busy health care professionals wanting to improve services and patient care. It is relevant to everyone involved in the organisation and provision of quality health care, including clinicians and health care managers, who are trying to lead change and improve care through implementing evidence-based guidance.
Gillian Leng, Deputy Chief Executive, National Institute for Health and Care Excellence, London, UK; Visiting Professor, King's College London, Division of Health and Social Research, London, UK Val Moore, Implementation Programme Director, National Institute for Health and Care Excellence, London, UK Sasha Abraham, General Practitioner, Tower Hamlets, London, UK
1 Introduction
Gillian Leng
Example in practice: Using clinical leaders to improve patient care
2 Practical actions for healthcare providers
Val Moore
Example in practice: A hospital wide approach to reduce mortality among acutely ill patients
3. Identifying a high quality evidence base
Paul Chrisp and Sara Twaddle
Example in practice: Finding a way through guidance on pre-hospital care across South West England
4. Key challenges to implementation and effective interventions
Elaine Whitby and Julie Royce
Example in practice: Changing behaviour in primary care to improve the management of children with feverish illness
5. Using financial systems to support improved care
Jennifer Field
Example in practice: Building a business case: To redesign diabetes services
6 Using measurement to support change and improvements in healthcare
Nick Baillie
Example in Practice: Setting up a service for peripheral arterial disease in the North East of England
7. Chapter 7: Conclusion and reflections
Danny Keenan and Sasha Abraham
Chapter 1
Introduction
Gillian Leng1,2
1National Institute for Health and Care Excellence, London, UK
2Division of Health and Social Research, King's College, London, UK
Introduction
Taking research evidence, interpreting it with input from patients and experts to generate best practice guidance is not straightforward. It is, however, relatively easy compared with the challenges of putting guidance into practice.
The National Institute for Health and Care Excellence (NICE) is very sensitive to this challenge as, since it was first established in 1999, over 900 individual pieces of NICE guidance have been published. These cover a range of topic areas, including the appraisal of new drugs, assessment of new diagnostic tests and other medical technologies, development of clinical guidelines and guidance for public health.
We know that simple dissemination of this best practice guidance is insufficient on its own to generate a change in practice. Indeed, this process could have almost no impact if the guidance is not seen to come from a credible, respected source. Evidence from the implementation literature indicates that no method for getting evidence into practice is effective, and that, to generate any change, efforts are required at national, organisational and individual levels.
The aim of this book is, at a very basic level, simply to help improve patient care through evidence-based practice. It takes a practical approach, starting with an overview of potential systems and processes for those providing health care, followed by more details on how to recognise high-quality guidance. This book then outlines some of the most frequently encountered challenges in changing practice, and suggests practical actions and financial mechanisms that might help overcome some of these challenges. Throughout the book, there are examples drawn from practice across the National Health Service (NHS), helping to bring to life some of the theoretical concepts.
Figure 1.1 shows the scope of this book, with each chapter expanding on a key part of the whole implementation process necessary to achieve high-quality care.
Fig. 1.1 Overview of process for achieving high-quality care.
What is the role of evidence?
The development of ‘evidence-based medicine’ as the underpinning approach to inform clinical practice is the approach that has grown and developed over a period of about 50 years. The history of using experimentation to confirm the effects of treatment goes back much further – one of the earliest clinical trials was conducted in 1747 by James Lind. He compared the effects of various acidic substances on sailors with scurvy and demonstrated that those given citrus fruits recovered after 6 days [1].
An expansion in the numbers of randomised controlled trials occurred rapidly in the 1950s and 1960s, increasing the body of evidence available to practitioners. This prompted Archie Cochrane to write critically about the lack of any systematic collection of research evidence in his 1972 publication, Effectiveness and Efficiency [2]. His criticisms spurred new, rigorous evaluations of health care interventions, and eventually led to the development of the Cochrane Collaboration in 1991.
There is no doubt that the methodology behind the rigorous development of systematic reviews has contributed greatly to an advance in medical knowledge. The research evidence base is seldom complete, however, as eloquently described by Lomas and colleagues: ‘Evidence is inherently uncertain, dynamic, complex, contestable and rarely complete’ [3]. This statement is illustrated in areas of medicine such as prognosis and diagnosis where there is relatively little research, and by the frequent absence of elderly patients with complex medical problems from randomised controlled trials.
The development of clinical guidelines provides a methodology to help overcome some of the issues generated by the variability in research evidence. Using a group process that facilitates input from relevant patients and experts, it is possible to generate a set of practical recommendations for practitioners informed by the best available evidence. This sometimes entails an extrapolation of the evidence, but the process also highlights gaps in the evidence with the aim of stimulating future research to answer key questions. The most sophisticated clinical guidelines, such as those developed by NICE, also incorporate an economic analysis alongside a review of the evidence on effectiveness.
A robust clinical guideline, therefore, represents a synthesis of the best available evidence, which has been interpreted by clinicians and patients to generate a set of practical recommendations. These recommendations, and the way in which they are phrased and presented, become key to stimulating a change in practice. They represent the ‘front face’ of the evidence, and must be sufficiently clear and concise to communicate the appropriate action required. Further details on the methodology of guideline development and how it helps drive implementation is given in Chapter 3.
How can guidance be used to track improvement?
The case for using guidance to inform clinical practice and improve patient care is a strong one. Assuming that the guidance has been developed using robust methodology, it will represent a statement of best practice informed by a comprehensive review of the evidence. Systematic use of this guidance will, therefore, have the benefits of
- ensuring that all practitioners are providing up-to-date care in line with the evidence;
- increasing standardisation of care across the country;
- improving access to new drugs and technologies that are considered cost effective;
- ensuring that patients benefit by receiving better care and by being informed about the treatments they should expect.
Guidelines represent one of the most important elements of evidence-based practice in health care. Clinicians often use them as stand-alone documents, but the recommendations are increasingly found embedded in electronic decision support systems where the doctor may not even recognise them as guidelines. The importance of using evidence-based guidelines is reinforced by medical defence organisations, which expect any variation in care from best practice guidance to be documented. Variation can of course be entirely appropriate – guidelines are not ‘rules’ – but it is important that a guideline is always considered, even if the recommendations are not then deemed appropriate in a particular individual.
Guidelines are often long documents, providing a comprehensive set of recommendations for a particular disease or condition. This is important in providing a complete overview of best practice, but can be challenging both in terms of identifying the most important areas for change and for tracking progress towards improvement. To support a focus on areas of improvement, NICE now uses guidance recommendations to generate a prioritised set of ‘quality statements’, which are concise, measurable statements designed to drive quality improvements across a pathway of care.
The benefits of prioritised quality statements are that they provide:
- a set of priority areas where improvements are most likely to be required;
- concise statements with associated measures and indicators to facilitate measurement of progress;
- a potential mechanism to incentivise improvements;
- a simple focus on high-quality care that is accessible to patients.
Where possible, quality standard statements will be associated with routinely measured indicators, with data collected and collated at a national level. This will greatly ease the burden of data collection at a local level. In other cases, measurement will require local audit, building on the well-recognised tradition of linking audit with guidelines. The benefits of audit in driving a change in practice will be covered later in this book.
What are the challenges to achieving quality improvement?
The concept of quality is a broad one and is generally recognised to mean either a statement of best practice (high quality) or a process of continuous quality improvement. A widely accepted description of quality across the NHS is probably the one defined by Lord Darzi in High Quality Care for All [4]. It describes a process of continuous quality improvement encompassing three elements: patient safety, clinical effectiveness and patient experience. NICE takes into account these three elements in producing guidance and setting associated quality measures. Sometimes, this description of high-quality care set out by NICE is aspirational and requires significant change to achieve.
There is no comprehensive mechanism, at a national level in England, for routinely tracking successful improvements that result from the adoption of NICE guidance recommendations. Wherever possible, NICE works with other organisations to gather as complete a picture of adoption as possible. This includes where NICE recommendations have been used in national audits and the analysis of routinely collected data that provides a proxy measure of impact.
In some cases, feedback demonstrates that new guidance has a rapid impact on practice such as in the prescribing of a new drug. In other areas, impact is much slower and, anecdotally, the reasons for this are often reported to be a lack of clinical leadership, a lack...
| Erscheint lt. Verlag | 29.7.2014 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Allgemeines / Lexika |
| Medizin / Pharmazie ► Gesundheitswesen | |
| Schlagworte | Barriers • Behind • Care • Change • concise • Evidence • Evidence-based Health Care • Evidenzbasierte Forschung im Gesundheitswesen • Excellence • Experience • Gesundheitspolitik, Risiken, Sicherheit des Patienten • Gesundheitswesen • Guide • Health • Health Policy, Health Risk & Patient Safety • High • Medical Professional Development • Medical Science • Medizin • national institute • New • overall • overcome • Overview • Patientensicherheit • Perspektiven in medizinischen Berufen • Picture • Practical • Practice • quality • successful initiatives • title |
| ISBN-10 | 1-118-54358-0 / 1118543580 |
| ISBN-13 | 978-1-118-54358-0 / 9781118543580 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich